I’ve done this 2 minute video with 6 quick tips about you can stay healthy and well this winter.
More to follow, but hope this helps!
I’ve done this 2 minute video with 6 quick tips about you can stay healthy and well this winter.
More to follow, but hope this helps!
 The Well is an extraordinary community of people. I respect them deeply and learn so much from every time I have the privilege of being with them, listening to their stories. They are all people on the journey of recovery from drug and/or alcohol addiction. They are welcoming, non-judgmental, caring, embracing and kind. Most importantly of all, they offer hope that no matter how far into hell you have been, there is a way out and no matter how badly you have messed up, you are lovable and worthy of a new chance. There are countless stories of those who have gone before, through the “12 steps”, and found transformational grace and and the chance of a new life. The support they give to each other, especially at times of trouble is based on openness, honesty, trust and
The Well is an extraordinary community of people. I respect them deeply and learn so much from every time I have the privilege of being with them, listening to their stories. They are all people on the journey of recovery from drug and/or alcohol addiction. They are welcoming, non-judgmental, caring, embracing and kind. Most importantly of all, they offer hope that no matter how far into hell you have been, there is a way out and no matter how badly you have messed up, you are lovable and worthy of a new chance. There are countless stories of those who have gone before, through the “12 steps”, and found transformational grace and and the chance of a new life. The support they give to each other, especially at times of trouble is based on openness, honesty, trust and a genuine love for each other that holds through difficult battles for a better future. Every story I have heard has humbled me, and each time I am with them, I go away changed and filled with fresh hope. I am so grateful that I can now count several members of the community as my friends. I feel we, as the medical community have much to learn from them.
a genuine love for each other that holds through difficult battles for a better future. Every story I have heard has humbled me, and each time I am with them, I go away changed and filled with fresh hope. I am so grateful that I can now count several members of the community as my friends. I feel we, as the medical community have much to learn from them.
 After my last meeting with The Well community, which was in Barrow In Furness, I then spent some time with an excellent Diabetologist, Cathy hay, who is employed by Cumbria Partnership Foundation Trust, but works at Furness General Hospital (another example of how we are breaking down boundaries and working more effectively as part of Better Care Together). I was learning from Cathy about how she and her amazing team are transforming how they care for and work with people who have diabetes. Like me, she believes that hierarchical behaviour gets in the way of building good relationships across teams, playing to each other’s strengths and working effectively with patients. She has worked hard to break down the ‘need’ for consultant follow-up clinics, putting the power back into patients hands. They have had a much more proactive approach at working with patients to really educate them and empower them about their own conditions through the fabulous work of the Diabetes specialist Nurses and Dietitians and a team of Psychologists, lead by Elspeth Desert, who help patients learn how to face up to and cope with physical health issues.
After my last meeting with The Well community, which was in Barrow In Furness, I then spent some time with an excellent Diabetologist, Cathy hay, who is employed by Cumbria Partnership Foundation Trust, but works at Furness General Hospital (another example of how we are breaking down boundaries and working more effectively as part of Better Care Together). I was learning from Cathy about how she and her amazing team are transforming how they care for and work with people who have diabetes. Like me, she believes that hierarchical behaviour gets in the way of building good relationships across teams, playing to each other’s strengths and working effectively with patients. She has worked hard to break down the ‘need’ for consultant follow-up clinics, putting the power back into patients hands. They have had a much more proactive approach at working with patients to really educate them and empower them about their own conditions through the fabulous work of the Diabetes specialist Nurses and Dietitians and a team of Psychologists, lead by Elspeth Desert, who help patients learn how to face up to and cope with physical health issues.
 Group programmes (such as DESMOND, DAFNE or the X-PERT courses) enable patients to build supportive relationships with one another and networks form in which patients are rightly able to become the experts in their own conditions, supported by a team of people who they can draw on, as and when needed – determined by the person with the condition. This cuts the need for outpatient appointments drastically and releases the team to work far more effectively. The ‘Walk Away from Diabetes’ programme encourages those with the earliest warning signs to try and avoid lifelong medication altogether through exercise, dietary changes and accountability with one another.
Group programmes (such as DESMOND, DAFNE or the X-PERT courses) enable patients to build supportive relationships with one another and networks form in which patients are rightly able to become the experts in their own conditions, supported by a team of people who they can draw on, as and when needed – determined by the person with the condition. This cuts the need for outpatient appointments drastically and releases the team to work far more effectively. The ‘Walk Away from Diabetes’ programme encourages those with the earliest warning signs to try and avoid lifelong medication altogether through exercise, dietary changes and accountability with one another.
 In some ways, the approach is similar to what I have experienced of The Well and it got me thinking about just how transferable this approach could be across health services, in an extremely timely and cost effective way…..(which although sounds potentially a little mercenary is actually really important – we do actually have a responsibility to use the resources we have as well as we can, and our previous models are no longer deliverable, given our financial and staffing pressures, let alone the increased numbers of people accessing services). What if, once people are diagnosed with a long-term condition, we give them the option of a self-directed, learning approach to their condition, in the context of community with others and a supportive network around them? We could save an inordinate number of unnecessary outpatient appointments. It puts people back in charge of their own bodies and conditions, far more empowered to make informed choices and enables care to be available in a more efficient, cost effective and timely manner. Communities of people, facing up to their conditions together, learning together, helping each other, supporting and resourcing each other and finding improved health and wellbeing at every level as a result.
In some ways, the approach is similar to what I have experienced of The Well and it got me thinking about just how transferable this approach could be across health services, in an extremely timely and cost effective way…..(which although sounds potentially a little mercenary is actually really important – we do actually have a responsibility to use the resources we have as well as we can, and our previous models are no longer deliverable, given our financial and staffing pressures, let alone the increased numbers of people accessing services). What if, once people are diagnosed with a long-term condition, we give them the option of a self-directed, learning approach to their condition, in the context of community with others and a supportive network around them? We could save an inordinate number of unnecessary outpatient appointments. It puts people back in charge of their own bodies and conditions, far more empowered to make informed choices and enables care to be available in a more efficient, cost effective and timely manner. Communities of people, facing up to their conditions together, learning together, helping each other, supporting and resourcing each other and finding improved health and wellbeing at every level as a result.
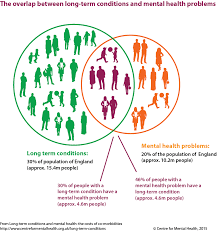 Many people across the UK have at least one long term condition. Many of these people also struggle with a mental health problem at the same time, often linked to the condition they live with. A more cooperative approach can break down some of the barriers and enable people to connect, which will improve both their physical and mental health at the same time.
Many people across the UK have at least one long term condition. Many of these people also struggle with a mental health problem at the same time, often linked to the condition they live with. A more cooperative approach can break down some of the barriers and enable people to connect, which will improve both their physical and mental health at the same time.
We are beginning to see an exciting redesign of our respiratory services along these lines, lead by Pat Haslam, Farhan Amin, Tim Gatherall, Shahedal Bari and the team……I wonder how brave we can be across the board and how much better our care might be together if we did?
services along these lines, lead by Pat Haslam, Farhan Amin, Tim Gatherall, Shahedal Bari and the team……I wonder how brave we can be across the board and how much better our care might be together if we did?
Tweet All this week on the BBC, there has been a focus on the NHS and the crisis we are in – don’t panic Mr Mainwaring…..There is a heady mix of opinions being thrown around – Question Time became quite a furore of ideas and thoughts last night – not enough beds, not enough staff, not [Continue Reading …]
Tweet It’s time to do the impossible. It’s time to turn the tide. In my last blog, I talked about the exponential potential of what could be possible if clinicians worked together in a more collaborative way. However, far more can be achieved if we work together in and with our communities to create a [Continue Reading …]
Tweet It’s all over our news today – our health is in a real mess, and this is our wake-up call moment – we really do need to take it seriously. It’s all very well us protesting about the under-funding and under-recruitment in our NHS (and we are right to do so), but we can [Continue Reading …]
Tweet My last blog focused on how we can think about solutions instead of problems in the NHS. Well the same is true in thinking about the health of our whole population. Yes there are some problems! We have growing health concerns with obesity and diabetes. We have huge health inequalities. There are major issues [Continue Reading …]
Tweet In my experience with patients I find two broad categories of people who live with chronic ill health (be that back pain, a life limiting condition like MS, COPD/Asthma/Diabetes whatever). Firstly, there are people who refuse to be shaped by their illness. They remain robustly determined that the illness will live with them but [Continue Reading …]