Last week Boris Johnson declared that we must do more to tackle Obesity, as the evidence has shown that it is a significant risk factor in increased mortality from Covid-19. Why it has taken this Coronavirus to wake the government up, I’m not quite sure, when we’ve known about the risk from obesity in terms of Type 2 Diabetes, Cancer, Musculoskeletal and Cardiovascular Disease for a very long time. However, the new strategy the government have released, is welcome, although it still puts too much emphasis on individual choice and fails to grasp some of the most important issues.
I’ve blogged on here previously about the complex nature of Obesity in our society. If we’re really going to tackle the issue of Obesity, we have to break the stigma of ‘fat-shaming’, undo the myth that it’s really just a simple matter of people ‘taking more responsibility, eating less and exercising more’ (see previous blog in which I draw on the phenomenal work of Prof Sandro Galea), understand the vast machine at work which is actually making us all more unhealthy and work out how we dismantle it and promote much greater wellbeing across society. There is no shame in being overweight. If everybody were slim and lithe, it would be very boring. However, being overweight (as indeed I am, currently) does lead us to have increased current and future health issues. With so many of us (67% of men and 60% of women) being over our ‘ideal’ BMI (body mass index) it’s causing us to live with more associated complexities and we do need to face this, however difficult it may be. We are told that Obesity is reported to cost £5.1 billion a year to the NHS…..But what does this mean to anyone except to induce more shame that their choices are costing the NHS and they should therefore change….it’s unhelpful and deeply demotivating.
This conversation cannot be about blame. It’s about examining the root causes. There are multiple levels of responsibility and complicity and so the answers are not simple, but are multifactoral. What I seek to do in this two-part Long-Read blog post is look at some of the deeper issues and where we might move forward into genuine solutions. This means owning up to mistakes and failures whilst finding a way forward together. What I do believe is that those who hold power and make decisions must take a greater share of this burden, rather than pushing it down onto the individual. On that basis, this blog-post will focus on all the other levels that can affect obesity and the following post will look at what individuals and communities can do/change in the light of this. I am not trying to give all the answers here. But I am trying to give a bit more provocation to the depth of debate and hope that we might take this conversation seriously.
Let us begin with National Government.
The National Government (particularly since 2010) has been woefully deficient in this entire situation. I say that, as the Marmot report highlights how inequality and health outcomes have worsened since that time. It has hidden behind the rhetoric of ‘free choice’, stubbornly believing that the ‘benevolent hand of the market’ will cause things to balance out. This libertarian approach is based on the notion that ‘the Nanny State’ is too interventionist and it is not the role of government to tell people how to live their lives. The government have turned a blind eye to corporate greed and irresponsibility, whilst blaming individuals for making poor choices, part of the ‘stigma machine‘ it has driven over the past decade to paint a picture of our poorest communities. Yet last year the food and drinks industry spent £143 million on advertising obesogenic products to the British public! As Shoshana Zuboff so powerfully demonstrates in her seminal work ‘Surveillance Capitalism‘, there is very little ‘free choice’ left in the world these days!
Johnson is perhaps waking up to just how fed up the nation is with ‘Austerity’, but many still believe that it was a ‘necessary evil‘ to dig us out of an economic black hole. It was a political choice. One that was unnecessary and one that has done great harm to the nation as a whole, but in particular to our most deprived communities, particularly when it comes to health outcomes. Tory Peers this week have shown just how inadequate ‘Universal Credit’ is, we continue to see a rise in the use of food banks (where healthy food choices are not altogether plentiful), fast rising admissions to hospital for children with malnutrition, falling life expectancy for women in our poorest communities, and significantly worsening obesity, again worse in areas of greater ‘deprivation’. All the while, the government pushed the responsibility for fixing this mess, primarily onto the individual but also onto local governments, through the realignment of public health in the coalition government reorganisation of the NHS. However, devastating cuts to these localities, meant a significant drop in public health spending. We’ve seen the loss of sure start, exercise programmes and healthy eating help (something the government is now wanting to replace, through a new scheme involving GPs).
It has taken Marcus Rashford to wake the government up to the effects of child hunger, though the summer holidays and further reports have shown just how inadequate the funding of schools is when it comes to tackling malnutrition. It’s a strange conundrum that obesity and malnutrition actually go together in our poorest communities. It’s all well and good telling individuals to get out and exercise, but with the loss of 21000 police officers, communities are now less safe, with many young children and teenagers unable to access local parks due to the associated increase in violent crime and gang crime, also linked with the loss of youth centres. Where are people supposed to exercise? In Morecambe Bay, a staggeringly high percentage of children in Barrow, have never visited the Lake District or even the beach! The same applies to Morecambe and Lancaster. Perhaps there is a solution, which I will come to later, but all this finger wagging, whilst cutting genuine accessibility due to poor transport networks, shows just how out of touch the government are with the effects of their own policies. Cutting theses services in the first place has made the health inequality gap widen.
On top of this, there has been almost no effective regulation of the sugar industry, which continues to pump more terrible calories into our food, without even telling us (and labelling hasn’t really helped, due to the ongoing power of advertising, BOGOFs and product placement). It’s important the government sorts out its own policies in this arena and its current proposals are not good enough, although they are at least a start in the right direction.
So, what does the government need to do?
1) It needs to ensure that Universal Credit actually works or consider a Universal Basic Income in its place. Poverty and Obesity are tightly aligned and current provision to tackle both is entirely inadequate. Until we see the demise of food banks, we will struggle to tackle the basics of health inequality. However, on current predictions, years of failed policies for our poorest communities will mean this will only increase as we enter a deep recession due to the double whammy of covid-19 and brexit.
2) It needs to stop the game of stigmatisation and the false blame of individuals. In her seminal work, ‘Stigma: The Machinery of Inequality’ (which I think is critical reading right now), Prof Imogen Tyler looks at how Stigma is weaponised by governments to inflict policies such as ‘Austerity’. These same mechanisms have been used when it comes to obesity and this kind of shaming must end.
3) It needs to get a grip of the Food (and in-particular Sugar) Industry. It needs to set tighter boundaries around advertising (good to see the beginnings of this in the new strategy), product placement and the content of sugar in products and stop hiding behind the nonsense of the nanny-state (again good to see a start on this by changing rules around advertising before the watershed). The Kingsfund (great work from David Buck) has clearly shown that people did not mind the intervention on smoking and would actually favour more government intervention in this field. The role of government, we are told, is to protect it’s people. There is so much more to do than the initial proposals being made.
4) The government needs to raise taxes on particular products, especially cakes and biscuits, to support nationwide behaviour change. Without this, it will be difficult to tackle ingrained behaviour. A century ago, chocolate was considered a luxury. We need to think of treats as exactly that and not a daily snack and price changes will cause this to happen better than almost anything else.
5) The government needs to put necessary protections in place for the Farming Industry and create legislation that moves us towards a more plant based diet, that is better for the human biome and tackles climate change, whilst also helping us to have healthier and more sustainable diets.
6) This may sound utterly controversial, but I believe may be a solution to help tackle both climate change and our health issues: they should consider rationing. We haven’t seen anything like this since WW2, but we’re in unprecedented times. If we are to ensure that everyone has enough and all people can eat well (therefore diminishing the need for food banks), whilst also helping us learn how to do so in a way that is not overindulgent, then this may be difficult but necessary medicine. How can we live in a world in which we throw away so much food, whilst millions go hungry? Would rationing help us to discipline ourselves and find a more sustainable and equitable future available to all? Heavy handed, I know, and probably laughable in some quarters, but maybe, during this pandemic, we should at least consider it – giving everyone a universal basic diet – I suppose it would be a bit like exploring a universal basic income – something which is gaining more support.
7) Central government must adequately fund local government, in particular public heath programmes and schools. The leader of Lancashire County Council has been clear with the Prime Minister, that the new allocation is well below what is needed for the task ahead. Does BJ have ears to listen? Do the government really understand the true power and nature of local governments and what they can achieve in partnership with the communities they serve? Look at what the Marmot Cities are beginning to achieve. Do we really want to stifle this? The healthy lifestyle programmes must be adequately funded and appropriately targeted towards areas with the greatest problems. They must also be designed in a way that encourages health rather than shaming ‘unhealth’.
8) The Government must take on the corporate giants. A few years ago, I started working with the Consumer Goods Forum (a network of manufacturers and retailers, with a combined global turnover over several trillion dollars) around how they might work more seriously in partnership with the NHS and PHE around the issue of obesity, diabetes and health inequality. I have to say that to date, although there is lots of willingness on paper, a combined effort is hampered by competition laws and the primary motivation of profit over all else. They could easily change product placement, especially at the tills; they could easily have been more on the front foot in helping us fight this crisis. Instead, they have tinkered around the edges, whilst raking in the profits. I hope now that they see just what obesity is causing in the complexities around Covid-19 that they might just finally take this a little bit more seriously and play their full part in changing this narrative. They say that they are simply meeting the demands of the public, and yet they are the ones who have spent colossal sums of money in advertising to convince us to buy products that do us harm and then pricing and placing them in a way that makes them utterly irresistible. I am therefore highly doubtful that they will change their behaviour unless forced to do so, which is why the government must be more interventional. Some of these companies don’t even pay their fair share of taxes, taking the profits whilst leaving the NHS to pick up the bill.
What Is the Role of Local Government?
I agree with Geoff Driver that the current promised funding for Local Government is terribly insufficient for the task ahead. However, with whatever package is finally agreed, there are certain things which I believe local councils must focus on. Firstly, they must take a collaborative approach WITH the communities they serve, building with and on community assets. Secondly, they must get a grip of local licensing of fast food restaurants and take-always – the current government proposals are unlikely to make much impact in inner city areas. Thirdly, they must invest in green and active transport, taking this opportunity to create many more cycle lanes and safe walking paths to ensure that they tackle both climate change and obesity in the same move. Finally, they must replace services they have cut and work in partnership with local NHS teams, especially primary care networks on the delivery of proven interventions.
The NHS
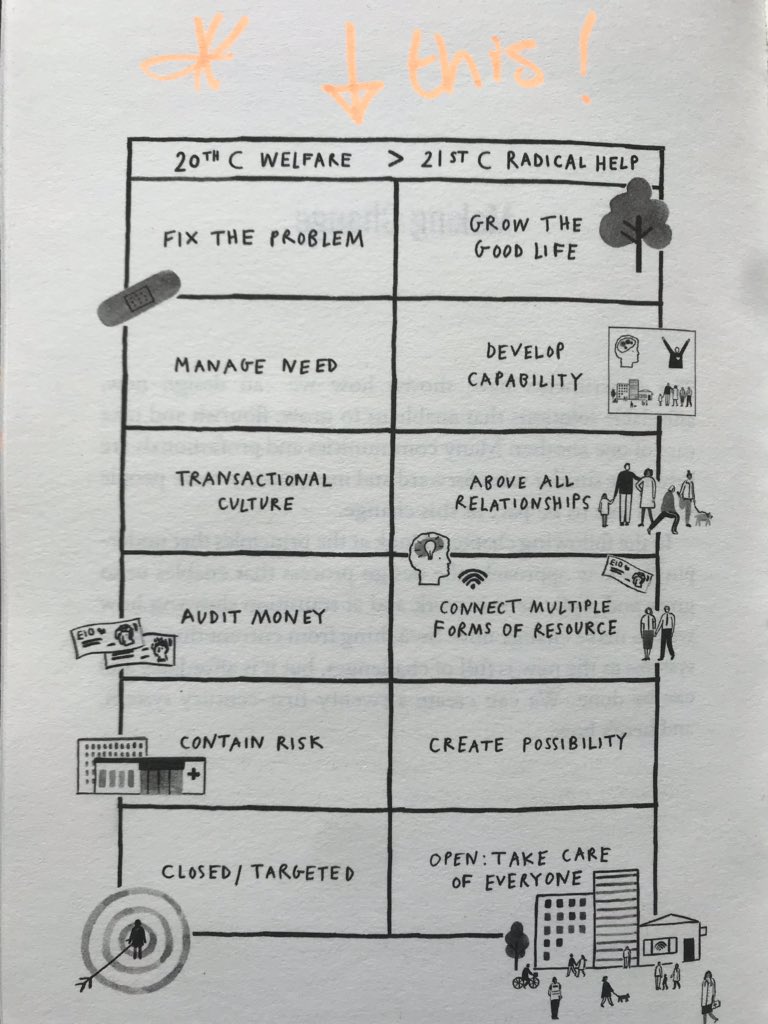
Some might think the NHS has quite a lot on its plate currently, but there is no doubt that it has an important role in tackling obesity. GPs and Practice Nurses have proven through great work around smoking, that they can make a significant difference as part of an overall strategy. However, given the complex nature of obesity, my recommendations would be as follows:
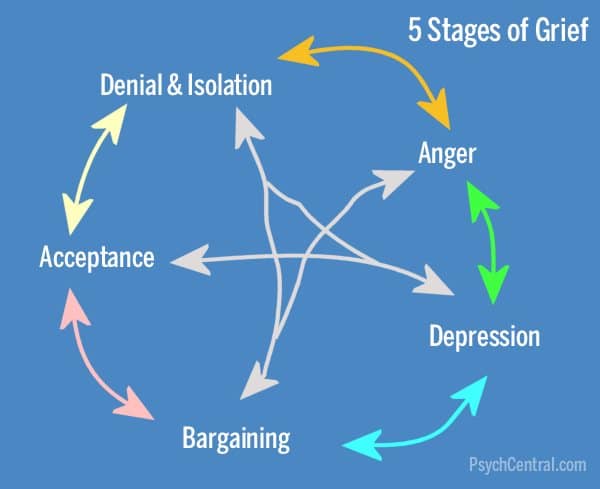
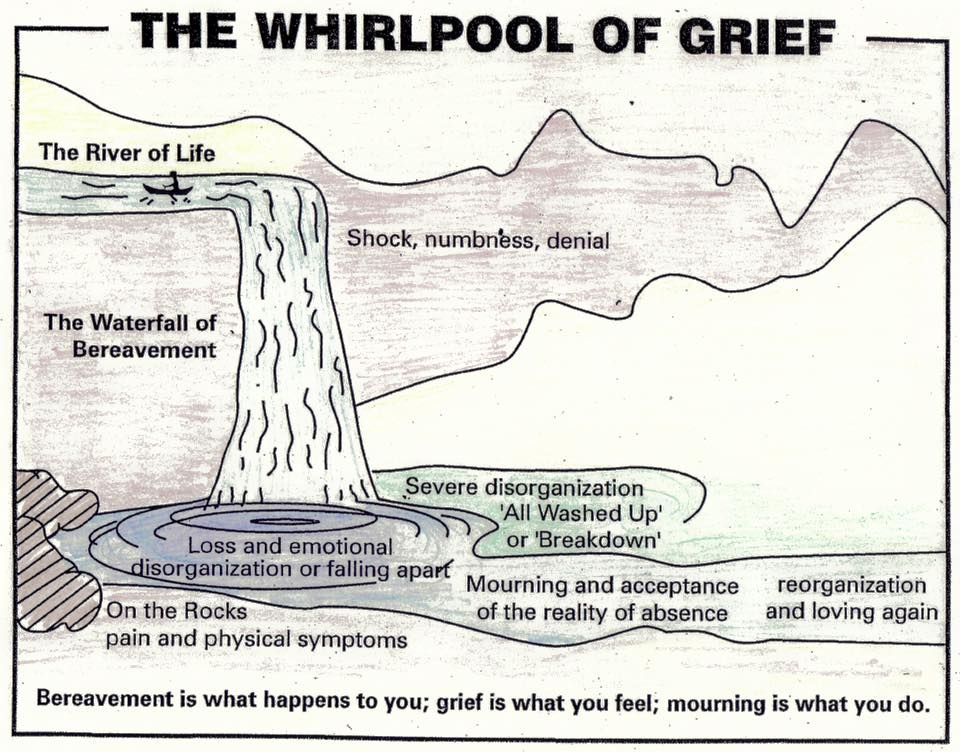
1) We need to talk much more about creating a trauma-informed approach. I would like to see the opening of ‘trauma-recovery centres’ in each of the regions of England and the other 3 nations. The reality is that obesity is massively linked to adversity experienced in childhood/adulthood and coping mechanisms associated with this. We need to stop asking people, ‘what is wrong with you?’ and be far more interested to find out ‘what happened to you?’ or ‘what is your story?’. Compassionate communities are those that recognise the complexity of our human lives and look at people with kind eyes, rather than judgement. It’s vital that this is more true than ever in the consultations room.
2) Leading on from this, we need to widen the use of ‘motivational interviewing’ and ‘coaching’ techniques, with help of the ‘patient activation measure’. We are using this with great effect in Morecambe Bay – it works with people so much more effectively than just telling them what to do. It enables people to feel empowered to make the changes they want to see in a way and a timescale that is realistic for them.
3) We must stop funding national programmes, which are ineffective (many of which are a total waste of time and money, in my opinion), and instead invest in helping PCNs listen to the actual needs of their community, through initiatives like the poverty truth commission, and then partner with those communities to bring about real, lasting, relational and effective change. If you compare what local PCN programmes are achieving around Type 2 diabetes reversal compared to the National Diabetes Prevention Programme (NDPP), which the government have given a further committment to rolling out, you would scrap the NDPP and invest far more in local communities, which are much cheaper and significantly more effective. Local relationships and expertise trump nationally driven campaigns every day of the week.
4) We have to look at the GP model and provision of care in our economically poorest communities. It has to be more attractive and we need to be braver at putting funding where it is needed the most. We won’t break down health inequalities, if we don’t get more clinicians working in and with those who are struggling the most.
5) We need to encourage better partnerships between GP practices and local schools in working towards a healthier place-based curriculum. We’re very blessed in Morecambe Bay to be working on this with the fabulous Eden Project North, but not everyone has this on their doorstep…..so what is possible in each locality?
6) Hospitals need to be doing much more with the money they are already given in making sure that ‘pre-hab’, prior to surgery is far more effective. I am aware of hospital trusts in which high percentages of patients are having routine knee and hip replacements, and routine abdominal surgery (like hernia repairs and cholecystectomies – gallbladder removals) with very high BMIs. Not only is this actually unsafe, it leads to much longer stays in hospital afterwards, driving up the overall cost the procedures. If hospital teams were dedicated to helping people achieve optimal weight before surgery, the number of people actually needing that surgery would dramatically reduce. We are currently implementing such a model in Morecambe Bay, thanks to a great partnership between GPs, Surgeons, Managers and Commissioners.
7) We need to see a faster integration of PCN teams to include Health Visitors and possibly, community midwives. The first 1000 days of a child’s life are vital at determining the course of the the rest of it’s long term wellbeing. Working with the ‘maternal commons’ and changing the tide for the future generations is vital. Things like Breast Feeding (which can reduce obesity by 25%!) and healthy snacks need to become the norm in all our communities.
Employers Have a Key Role!
The work place environment is often incredibly unhealthy. However, we have learned together, through this current pandemic, that it really is possible for us to work differently. Greater workplace flexibility to encourage exercise breaks, healthy eating in the work place and active travel should now become routine parts of the day. It makes total economic sense. A happy and healthy workforce are more likely to stick with a company and have less time off sick. It’s absolutely vital that we end ‘in-work poverty’ by seeing a true living wage across the UK. It’s one of the reasons I am so passionate about seeing the NHS as an anchor institution in each area through the UK, partnering with other organisations to set the standard of good employment. The new NHS people plan sets us firmly in the right direction.
National Parks/The National Trust/Areas of Outstanding Natural Beauty
I would love to see an agreement between the department for education, local governments and these national treasures to become much more widely available to children from our poorest communities. These places are primarily now the playgrounds of the middle-class only, but this is unacceptable. How can we ensure that all our children can enjoy the delights of the counties across the UK, and not just the privileged few? How can we make it more affordable for communities to get to these places, pay the entrance fee (where warranted) or believe that they are really for them? The National Trust was set up for the poor…..can it rediscover what it exists for?
Schools
Schools are underfunded and teachers are underpaid – let me just put that out there, before making any recommendations. The amount that teachers are now having to deal with in their classrooms around hunger alone, is beyond unacceptable. Children in our poorest communities are eating highly processed and insufficiently nutritious food, leaving them both overweight and malnourished simultaneously. We desperately need to build a curriculum around food security and physical and mental wellbeing. The focus is currently wrong and we are punishing children who are too hungry to learn. We must also think creatively about the timetabling of Physical Education, especially for our young women. The link between maternal obesity and the child’s future poor cardiovascular health is staggering. I recently did some listening with some teenage young women, who told me plainly about the jeering they continually get from boys when in their PE outfits, the horrors of having PE in the first period and then feeling red and hot and sweaty all day and therefore the high numbers of ‘drop-outs’ from PE lessons. Exercise is such a vital part of life, helps us focus on our work and have better mental health outcomes. Given the crisis we are facing, both around mental and physical wellbeing in our schools, is it time to radically rethink the school uniform, the PE ‘offer’ and how we might move towards a more inclusive and less ‘macho’ PE culture? Alongside this, we need to look at the quality of school meals – surely we can do better?!
Conclusion
The current narrative around obesity is full of stigmatisation and is grossly oversimplified. I hope that this blog has highlighted some of the complexity involved and therefore why we should approach the discussion with more humility and compassion. Of course individual people and communities have a role to play in the choices they make and the behaviours they adopt (and in my next blog, I will give more thought and focus to this), but for too long, we have made that the focus and forgotten about the enormous environmental factors which have caused the situation we find ourselves in. We will have to see just how serious the government is about really addressing the health inequalities in our nation. Obesity is a good ‘test-case’ and will mean a major sea change in policy and implementation at every level of society. I hope this blog goes some way to stimulating even more debate about how we break the stigma of obesity and find solutions which genuinely change the outcomes for Marmot 2030!