I’ve been thinking about how people can best use their time, if they are stuck at home during this Corona Virus, Covid-19 Pandemic. Some people will be asked to ‘self-isolate’, along with their household for 14 days because they have symptoms of a high temperature and/or a persistent and troubling cough. Others will be asked to do the same for 12 weeks if they are pregnant, over 70, or usually receive a flu-jab on the NHS (due to having an underlying health condition or on medication that suppresses their immune system). The reason for all of this is to try and suppress the spread of this virus, and maintain health in the wider community until we are sure we have better treatments and a vaccine that we can use across the population. Obviously, if you’re unwell, the first priority is to give your body time to recuperate by taking plenty of fluids (2-3 litres of water per day), eating well, sleeping and letting your immune system do it’s job, whilst you take paracetamol (at the recommended dose) to control your temperature and levels of pain. For many people, however, this time may feel frustrating, because symptoms will be mild or absent and some will be wondering what to do with the time they have been ‘gifted’.
There are 4 things, which I believe we can all do during this time, if we find ourselves in the situation of being in isolation, but not actually feeling too unwell.
- REST
- REFLECT
- RE-IMAGINE
- RESET
This is something which we tend to not be very good at. However, we have been given the opportunity to step back from the fast-paced, consumerist-approach that we have adopted in society and take some time to just BE. Learning to accept that we are where we are and deliberately slowing down will enable us to find new strength and reconnect with that which is most important. Deliberately slowing down our breathing, our pace of walking and learning to calm our racing thoughts allows us to enter into a different mindset. Choosing to turn off our screens and disconnect from social media for good portions of the day allows us to create space in our heads and our hearts for another way of being. I know that social media can be a really important and safe space for many people to continue to connect and feel part of community, breaking down a sense of isolation and loneliness, but if we’re on there all the time, it can really fill our heads with unhelpful traffic and noise, which stops us being able to enter rest. As we rest, we are invited to spend our time differently – to do things that are good for the soul. You could take time to create, write, read, sing, dance, pray, go for a gentle walk, cook, sit round a table and build Lego or do jigsaws with others or on your own. There is no need to accumulate new things, what can you make do with or mend? What old or new hobbies might you rediscover or pick up? How about deliberately choosing not to get a thousand and one jobs done around the house or not rushing into a new decorating project. Just stop for a while, slow-down and rest.
When we consider the far reaching potential effects of a global pandemic, like the one we find ourselves in, it causes us to pause, notice more the interconnectedness of human life across the world and the utter fragility of our systems. It should cause us to notice more deeply the injustices upon which we build our society, the insecurity of work and the implications of global capitalism on the poorest in our communities and indeed our environment. During this time, we do well to reflect on what we are learning together. Birds are heard singing for the first time in years in Wuhan – a city usually thick with smog. Destructive air pollution has reduced by over 25% in China and Italy. The canals are cleaner than ever in Venice and global air travel has decreased significantly. Of course, we notice some of the worst bits of our humanity – driven by fear – and some selfishness. But we also see the indomitable human spirit at work – huge acts of love, courage, kindness and generosity. There are amazing offers to help and support with home schooling and teachers are going above and beyond their usual brilliance, thinking creatively about how best to enable their students to thrive. Healthcare workers continue to put themselves at risk and pour themselves into the work of healing. Voluntary food clubs to feed the hungry, delivery services for shopping and medication, community support schemes and the ongoing service of the most vulnerable in our society – it’s amazing. This ability to re-organise ourselves, to connect together differently, to make wider political and economic decisions and find a way to be that feels more wholesome should give us plenty not only to be grateful for but to reflect on about why we put so much energy into maintaining the usual status quo. What good things are we noticing and learning?
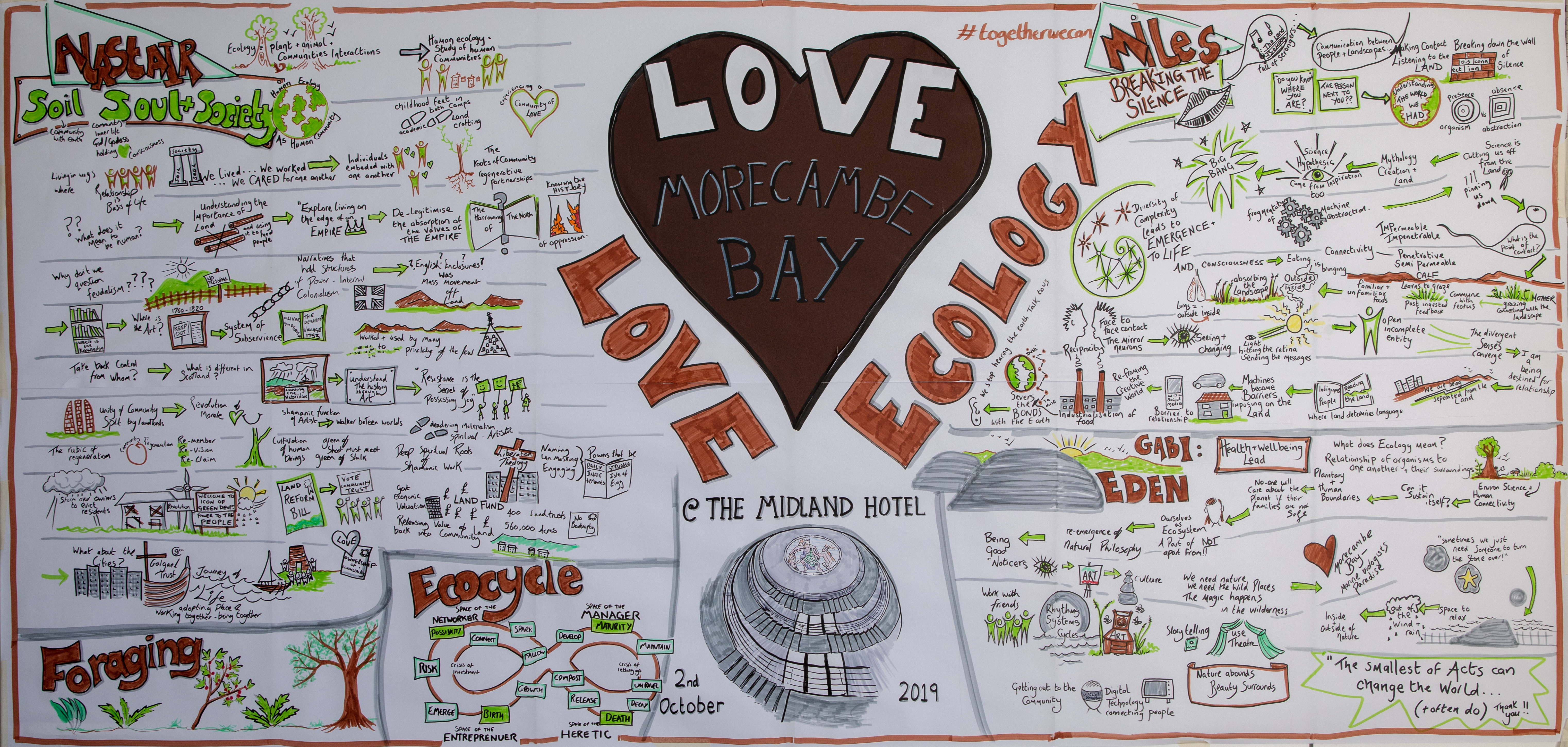
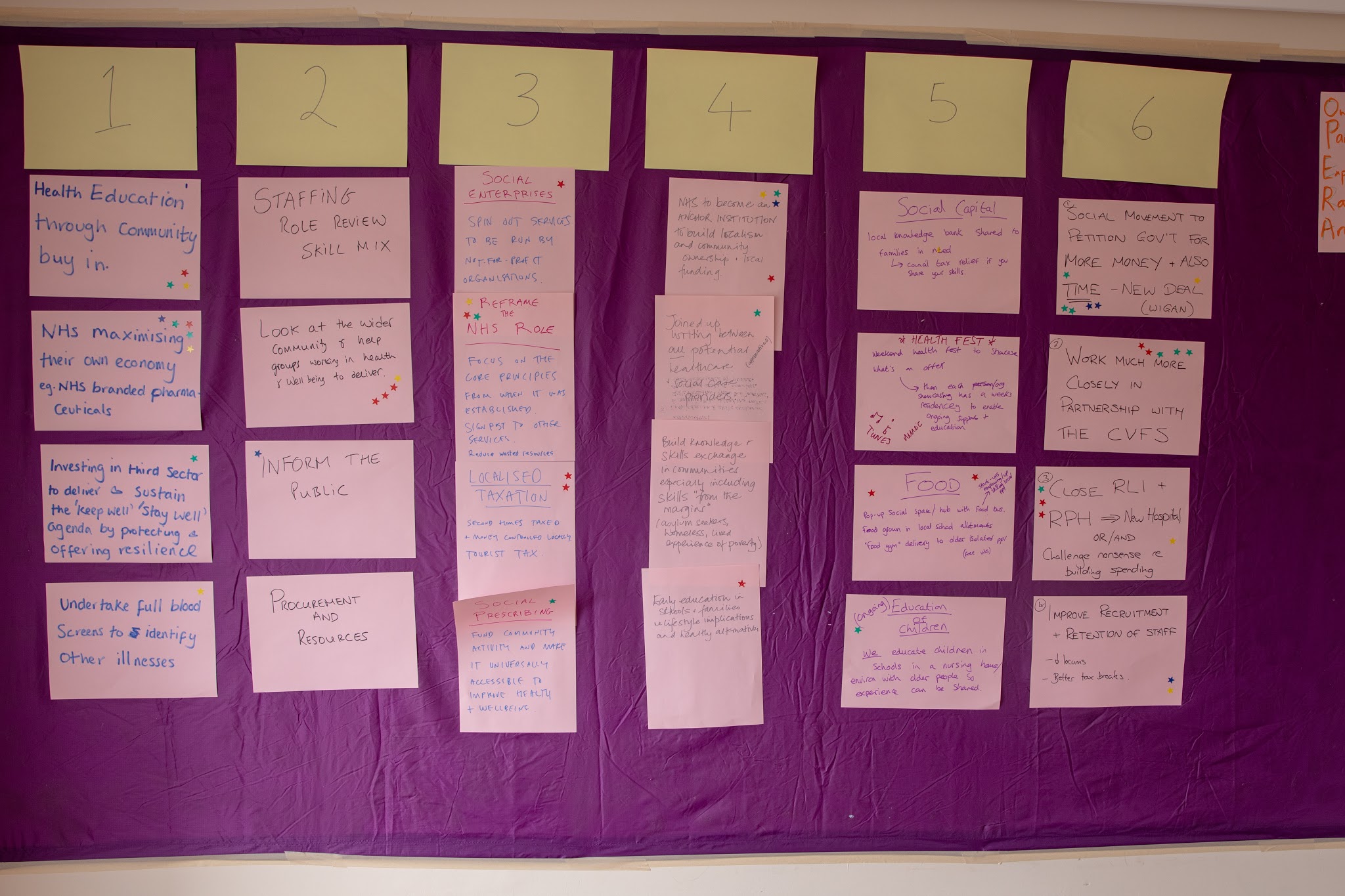
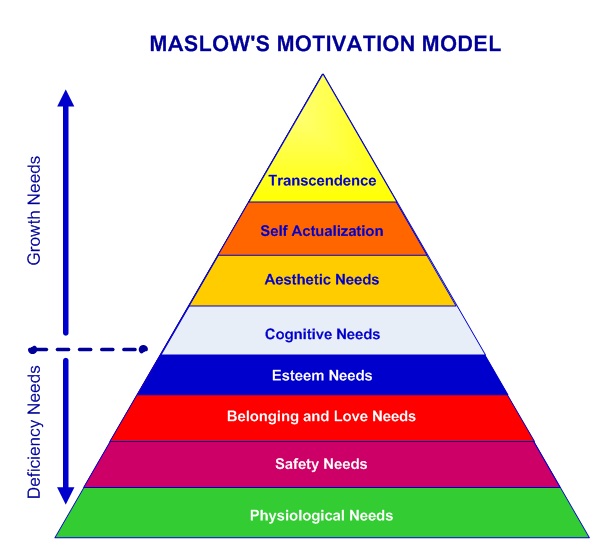
What might be possible together? Can we imagine a world with less commutes and more digital connection? Doesn’t it seem more possible to cut global emissions a great deal more quickly, when we’re forced to focus our attention? Could we work and earn differently and be more generous with wages and leave, so that we don’t see so many people left in such a vulnerable state. If we can find the ability to be so kind to each other at such a time as this – why not more so all the time? As we’ve recognised the fragility of our lives and existence, are the grudges we hold worthwhile? Are we able to forgive and reconnect? Might we adopt a way of life that is more about sharing and regenerating than grabbing all we can? Isn’t community one of the most delicious and richest of experiences? How can we build more of it? Can you sniff an economics that is more about wellbeing than profit and a politics that is more about connection and participation in our life together than centralised sovereignty? How about an education system that doesn’t treat our children like fodder for the machine, but invests in their ability to build a beautiful future. Have you seen how relationship really could be the foundation of our public services? So how might we think differently about our governance structures and the way we organise ourselves – think ‘Radical Help’ (Hilary Cottam), ‘Doughnut Economics’ (Kate Raworth) and ‘All Our Welfare’ (Peter Beresford) – plus many more. Can you imagine a society in which we really put the wellbeing of all people and the planet at the heart of what we do? If so….why would we continue with a way of being together which is so detrimental to both?
Our invitation, therefore, is to reset. This invitation comes from the earth itself, from our deepest longings, and from the source of all love and life itself. We don’t have to continue living in the story of selfishness and scarcity. We have shown ourselves that there is a more ancient and wonderful story of connectedness, restoration and hope, to which we all belong. We don’t have to go back to how it has been. Step by step, we can use this ‘kairos’ moment to walk into a new future together. A future in which we heal our divides and regenerate our planet, forgive our deep, historical wrongdoings, rebuild our ruins and restore our relationships; do away with injustice and create reconciliation. It’s time to reset. Are you ready to press the button?
Here is a beautiful poem, by Kitty O’Meara, to help us rest, reflect, re-imagine and rest.