*Warning – this blog contains swear words (not that I’m usually a potty mouth!)
This last week we had a gathering of clinical leaders around Morecambe Bay – Nurses, Occupational Therapists, Health Visitors, Midwives, Doctors, Surgeons, Physiotherapists, Pharmacists etc. We were gathered from across primary and secondary care to look together at the financial deficit we are facing as a health community across the Bay where we are seeking to serve our population.
The debt we’re facing (a hole of around 38 million of our English pounds!) is no small thing. Most of it is historic and much of it had nothing to do with us. I spent my first eighteen months as a commissioner feeling furious at the government. I wanted to rail against the machine, the injustice of working in such an oppressive, top down and hierarchical system, which feels like being among the Hebrew Slaves in Egypt when they were told to make the same number of bricks with less resource available to them. I felt so angry with the fact that we invest so little of our GDP into health and social care compared to similar countries and when further unthought through policies were dictated from Whitehall, I felt a total rage. It doesn’t help being politically pretty far to the left and working under a regime to which I feel ideologically opposed.
But one day, I realised two things. The first thing I realised is that the government are not going to change their position or policy. Our systems of government are not set up in a relational, collaborative or solutions focussed way. It doesn’t have to like this, but this is the way it currently is. Our systems have become the very antithesis of their purpose. Rather than serve the needs of the people, the people now serve the systems. The second thing I realised was that my anger didn’t achieve anything except to make me feel tired, disempowered and stressed. I had retreated into the less healthy parts of my personality in which I was keeping false joy alive and feeling burnt out in the process.
Truth has the ability to set you free. When we face truth, no matter how painful, it gives the choice of being more free. Facing up to the truth that the government are not about to change their modus operandi and that I was feeling angry and stressed allowed me to step out of rather childish thought processes and step into something altogether more wholesome. It allowed me to step out of a false sense and rather oppressive noun of responsibility and gave me the space to think more creatively about how I am part of a community of people who can respond to the situation we find ourselves in. We can respond (verb) once we step out of the oppressive yolk of responsibility (noun).
So, those of us in clinical leadership may have not created the financial situation, but there are some stark realities for us to face up to. Whether we like it or not, our current ways of working carry much waste, caused partly by the way the finances of the system operate, but also because we have not thought of ourselves as one. There are ways we behave within the system that create more financial problems and do not serve the community as well as we could. And so it is time for us to do what we can, within our gift by being much braver in our approach. I am suggesting that there are three Cs that are vital to our future.
- Collaborative
 We need to reimagine ourselves as all being part of a team who are together tackling the health crises we are facing. We know only too well that, as just one example among many, we are failing kids with asthma because we have not joined up our resources or thinking adequately enough. Yes there are major issues with housing, smoking and pollution, but let’s not point the finger or push the problem somewhere else. Let’s use the phenomenal brains God has given us to pull the right people round the table and work out what we’re going to do about it. Let’s change the way we spend our time so that we’re in schools, we’re listening to our communities and we’re partnering together outside of our normal comfort zones to change the health of the generations to come. We know only too well, that if we don’t shift our focus towards population health and work more intentionally with our communities, doing things with them rather than too them, we will never win this battle. We’re not about playing political games. We are about working with our communities to create optimal health for every person no matter who they are or where they are from. We need to be braver, push the boat away from the shore we know and face the uncertain waters of working altogether differently. In my next blog I will explore some of the possible ways we could work differently.
We need to reimagine ourselves as all being part of a team who are together tackling the health crises we are facing. We know only too well that, as just one example among many, we are failing kids with asthma because we have not joined up our resources or thinking adequately enough. Yes there are major issues with housing, smoking and pollution, but let’s not point the finger or push the problem somewhere else. Let’s use the phenomenal brains God has given us to pull the right people round the table and work out what we’re going to do about it. Let’s change the way we spend our time so that we’re in schools, we’re listening to our communities and we’re partnering together outside of our normal comfort zones to change the health of the generations to come. We know only too well, that if we don’t shift our focus towards population health and work more intentionally with our communities, doing things with them rather than too them, we will never win this battle. We’re not about playing political games. We are about working with our communities to create optimal health for every person no matter who they are or where they are from. We need to be braver, push the boat away from the shore we know and face the uncertain waters of working altogether differently. In my next blog I will explore some of the possible ways we could work differently.
2) Clinical
In order for the NHS to adapt and become sustainable for the future, we must not be afraid of clinical leadership. Our managers have a phenomenal set of skills, which we must draw on, but there is a trust we have amongst the communities we are embedded in that means they will trust us, if we engage with them properly that will allow us to turn this ship in a new direction. We must partner with our managerial colleagues, but be braver about the direction in which we know deep down we need to head in. We have gained so much expertise and trust and this is not a time to waste it or bury our heads. We must be braver and bolder in our vision of what we can really achieve together.
3) Community
 As clinicians we must, as many have stated this week, build bridges not walls. There is far too much division, suspicion and competition amongst us. (Here comes the swearing)…..I was in a conversation with a consultant colleague recently and he was relaying to me that another consultant referred to GPs as a “bunch of Fuck Wits”. In a separate conversation, one of my GP colleagues referred to consultants as a “bunch of arrogant Shits”. These kind of attitudes pervade the NHS and have created a culture of dishonour, distrust and division. Honestly! We’re better than this. How are we going to create the new workforce of the future that works across our currently artificial boundaries if we don’t teach them basic respect? This week a patient came to see me because he was dismayed at having to have seen a nurse at the hospital after suffering a significant condition and wanted to check that I, as a doctor, was happy with what he had been told. I could have laughed it off, but I wanted to stand up for my nursing colleague, who actually has far more expertise in this area of medicine than I do. The advice he had been given was perfect and completely in line with the best guidance available. We must not be afraid to challenge attitudes that are antiquated and out of place. More than ever, we need a culture of honour. A culture of honour is one in which we believe the best of each other, speak well of each other and appreciate our brilliantly necessary but differing gifts and expertise. We need to work out how we work effectively together for the best of the people we serve. We need to connect with each other and rehumanise the system in which we work. When was the last time you met as a cross cultural or multidisciplinary team and simply told each other what you love and appreciate about each other and the work you do? If we can’t learn to be more relationally whole, we will continue to work in the midst of serious dysfunction and strife. Come on – amongst us we have some remarkable gifts of wisdom, healing and hope. Let’s build the kind of culture and community amongst us that stands shoulder to shoulder, changes the story in the media and speaks with one voice to the powers that we are about the a new way of working together through relationship not hierarchy and fear. What might we really achieve together? It is this kind of collaborative clinical community that can change the future of healthcare, not just in the UK, but right across the globe.
As clinicians we must, as many have stated this week, build bridges not walls. There is far too much division, suspicion and competition amongst us. (Here comes the swearing)…..I was in a conversation with a consultant colleague recently and he was relaying to me that another consultant referred to GPs as a “bunch of Fuck Wits”. In a separate conversation, one of my GP colleagues referred to consultants as a “bunch of arrogant Shits”. These kind of attitudes pervade the NHS and have created a culture of dishonour, distrust and division. Honestly! We’re better than this. How are we going to create the new workforce of the future that works across our currently artificial boundaries if we don’t teach them basic respect? This week a patient came to see me because he was dismayed at having to have seen a nurse at the hospital after suffering a significant condition and wanted to check that I, as a doctor, was happy with what he had been told. I could have laughed it off, but I wanted to stand up for my nursing colleague, who actually has far more expertise in this area of medicine than I do. The advice he had been given was perfect and completely in line with the best guidance available. We must not be afraid to challenge attitudes that are antiquated and out of place. More than ever, we need a culture of honour. A culture of honour is one in which we believe the best of each other, speak well of each other and appreciate our brilliantly necessary but differing gifts and expertise. We need to work out how we work effectively together for the best of the people we serve. We need to connect with each other and rehumanise the system in which we work. When was the last time you met as a cross cultural or multidisciplinary team and simply told each other what you love and appreciate about each other and the work you do? If we can’t learn to be more relationally whole, we will continue to work in the midst of serious dysfunction and strife. Come on – amongst us we have some remarkable gifts of wisdom, healing and hope. Let’s build the kind of culture and community amongst us that stands shoulder to shoulder, changes the story in the media and speaks with one voice to the powers that we are about the a new way of working together through relationship not hierarchy and fear. What might we really achieve together? It is this kind of collaborative clinical community that can change the future of healthcare, not just in the UK, but right across the globe.
 We often talk about physical, mental, social and even systemic health, but we don’t often think or talk about the health of our personalities. Our personalities are shaped by our self-esteem, our values, our truths, our needs, our struggles, our instincts and our gifts. They impact every part of our lives, relationships and interactions with the world at large and although we give some focus to understanding them through tools like Myers-Briggs, the Enneagram and Strengths-Finder, (perhaps to make us more successful), we give little thought to how healthy we are when it comes to this subject.
We often talk about physical, mental, social and even systemic health, but we don’t often think or talk about the health of our personalities. Our personalities are shaped by our self-esteem, our values, our truths, our needs, our struggles, our instincts and our gifts. They impact every part of our lives, relationships and interactions with the world at large and although we give some focus to understanding them through tools like Myers-Briggs, the Enneagram and Strengths-Finder, (perhaps to make us more successful), we give little thought to how healthy we are when it comes to this subject.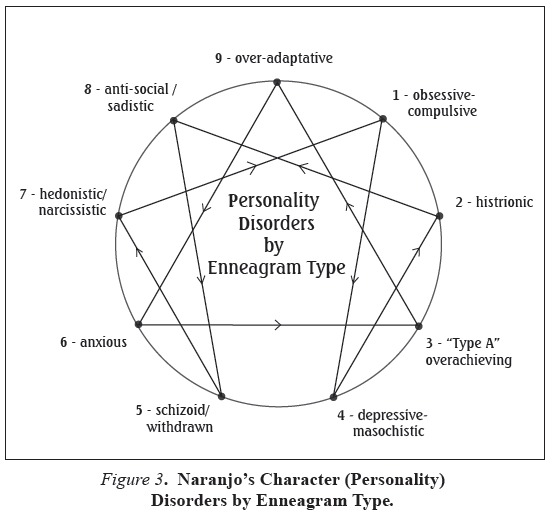 Now, what is particularly interesting to me as a doctor are 2 things related to this. Firstly, our personality type is hugely linked to the kind of mental health problems we might be more likely to develop. I wonder how often clinicians see the presentation of a mental illness and are able to talk with the person in front of them about which aspects of their personality might need therapy in order to help their mental health improve? As the whole area of positive psychology develops, it is vital that there are learning environments in which clinical teams can learn about innovative approaches in psychology that avoid the over prescribing of medication, especially in our younger population.
Now, what is particularly interesting to me as a doctor are 2 things related to this. Firstly, our personality type is hugely linked to the kind of mental health problems we might be more likely to develop. I wonder how often clinicians see the presentation of a mental illness and are able to talk with the person in front of them about which aspects of their personality might need therapy in order to help their mental health improve? As the whole area of positive psychology develops, it is vital that there are learning environments in which clinical teams can learn about innovative approaches in psychology that avoid the over prescribing of medication, especially in our younger population. The second area of interest is to do with how we can be more self-aware of how healthy we are or when we have reached a point at which we can no longer really help ourselves but need others who love us or care about to to intervene. Below is a chart (of sorts) which I learned about during a weekend on the Enneagram. It helps to explain aspects of personality health. I recognise that at times I am functioning more healthily than at other times, due to a combination of internal and external factors. I think there are behaviours we can be aware of, or ways in which we are operating in relationships and situations which should serve as a WAKE UP CALL to us. When we notice more negative patterns, we need to take stock of where we are and work out our lines of responsibility to help us back into a more healthy state. However, if we don’t, things can continue to worsen until we reach a point at which we need others to intervene on our behalf and rescue us from our self-destructive and damaging sickness.
The second area of interest is to do with how we can be more self-aware of how healthy we are or when we have reached a point at which we can no longer really help ourselves but need others who love us or care about to to intervene. Below is a chart (of sorts) which I learned about during a weekend on the Enneagram. It helps to explain aspects of personality health. I recognise that at times I am functioning more healthily than at other times, due to a combination of internal and external factors. I think there are behaviours we can be aware of, or ways in which we are operating in relationships and situations which should serve as a WAKE UP CALL to us. When we notice more negative patterns, we need to take stock of where we are and work out our lines of responsibility to help us back into a more healthy state. However, if we don’t, things can continue to worsen until we reach a point at which we need others to intervene on our behalf and rescue us from our self-destructive and damaging sickness. function healthily. However, through a mixture of internal and external factors, our hearts can become less healthy. When this occurs, our body will fire some warning shots to us, giving us a chance to change before something more serious occurs. This might be signs and symptoms do do with our weight, nutrition, fitness, level of breathlessness, vague chest pains, markers in our blood tests – like high cholesterol and high sugar, rising blood pressure etc. However, if we ignore the opportunities to change and continue with our unhealthy choices, eventually we will reach the point at which we have a significant event, e.g.the start of angina, a heart attack, a stroke, the development of diabetes. At that point we need the help of someone else – we can no longer do it on our own. Of course, we still have choices and can reject the help on offer, but if we do, we risk our own demise and ultimate death.
function healthily. However, through a mixture of internal and external factors, our hearts can become less healthy. When this occurs, our body will fire some warning shots to us, giving us a chance to change before something more serious occurs. This might be signs and symptoms do do with our weight, nutrition, fitness, level of breathlessness, vague chest pains, markers in our blood tests – like high cholesterol and high sugar, rising blood pressure etc. However, if we ignore the opportunities to change and continue with our unhealthy choices, eventually we will reach the point at which we have a significant event, e.g.the start of angina, a heart attack, a stroke, the development of diabetes. At that point we need the help of someone else – we can no longer do it on our own. Of course, we still have choices and can reject the help on offer, but if we do, we risk our own demise and ultimate death. My point is this. If we do not take the health of our own personalities seriously, there are serious and significant consequences, not only to ourselves but those around us and the world we live in. Many of us reach a point when we need help, but might not even face up to this, due to the poor health we are in. In those times, we need those who love and trust to be brave enough to reach in and offer us a life line. We may have even reached the place where we need resuscitation, when all our pride has gone. When we have ignored the red flag, we need those around us who will risk our total rejection of them to love us enough to offer us a way back to health. We need to take the health of our personalities seriously – it actually has a huge bearing on all the other aspects of our health. We also need
My point is this. If we do not take the health of our own personalities seriously, there are serious and significant consequences, not only to ourselves but those around us and the world we live in. Many of us reach a point when we need help, but might not even face up to this, due to the poor health we are in. In those times, we need those who love and trust to be brave enough to reach in and offer us a life line. We may have even reached the place where we need resuscitation, when all our pride has gone. When we have ignored the red flag, we need those around us who will risk our total rejection of them to love us enough to offer us a way back to health. We need to take the health of our personalities seriously – it actually has a huge bearing on all the other aspects of our health. We also need