I recently wrote a blog about reimagining health and care in this apocalyptic moment. In this post, I want to put a bit more flesh on the bones of what that might actually look in the context of the NHS, here in the UK and particularly, England.
Let me just make a few statements about where I’m at when thinking about future health and care:
I believe in a publicly funded and provided national health and care service, paid for through fair taxation.
I believe that health and care should be available to all people, equally, regardless of ability to pay.
I believe in locally led health and care systems, embedded in local communities.
I believe prevention is better than cure and we need to get up stream and stop people falling in the river in the first place.
I believe creating great working cultures enables teams to flourish and brings out the best in people. I know right now that our health and care workforce is feeling burnt out and overwhelmed. We can’t keep working under the huge burdens of constantly changing goal posts, key performance indicators and heavily mandated targets. The wellbeing of those who work in this sector has been overlooked for too long and the stress levels caused by the sheer pace and volume of work are not acceptable.
I believe there is systemic and ingrained racism in our communities and within the NHS and even though I consider myself to be ‘woke’ about this, as a privileged, white, male, there is still so much work for me and us to do, both internally and externally in order to break the curse of white supremacy. It is simply not enough to say ‘black lives matter’ – our words are cheap unless we do not confront internalised narratives and change society together, from the inside-out through truth and action.
I believe our economic system is no longer fit for the 21st century and am so grateful for the reimagining of what economics is for.
I believe the role of government needs to radically change to be much more empowering of local communities, with appropriate frameworks to support this. We are seeing the mess of centralised control, with unchecked and wasteful investment in the private sector, rather than local community empowerment in this current Covid-19 pandemic.
I believe communities are able to self-organise phenomenally well, as we have seen throughout this pandemic and should be supported to do so more through a much more participatory and relational politics.
I believe that any health and care service should promote overall wellbeing by paying extra special attention to:
- instating women fully and equally
- prioritising children
- advocating for the poor and breaking down health inequalities especially through challenging stigma (Very grateful to Imogen Tyler for her great work on this)
- welcoming ‘strangers’ (by this I particularly mean the way we treat staff from overseas and how we care for refugees and asylum seekers)
- reintegrating humanity with the environment (e.g. by getting back to basics of nutrition and sustainable food)
- restoring justice to prisoners (metaphorical and real)
- healing the sick – through both slow and fast medicine
- ensure the honouring the elderly In how they are cared for
So……(!)……How do we take the best thinking around health and care systems and make it real and practicable in the NHS and Care System? Firstly, I suggest that we need to take the hierarchical, pyramidal system and simply flip it upside down. Let’s begin at the local level, as the foundations stones of a reimagined health and care system and build from there. With this we need to take seriously what Simon Parker is calling for in a rethink of what government exists for.
Within the health and care system though, we don’t another fresh reorganisation. We have some good things we can play around with. We just need to stretch our thinking a bit more and permission some creative, entrepreneurial experiments and we can see something really exciting emerge. Primary Care Networks are a good basic building block, which take the best of clinical leadership, and when done properly, combine it with local communities to build local health and wellbeing. They cause General Practice to work together more collaboratively, use the best of available data to map the issues a population are facing and have the flexibility to begin working differently. They are not perfect, and in my opinion, need some adaptation, if they are going to enable the tackling of health inequalities, social injustice and true community empowerment.
Firstly, they need more time. The phrase ‘at pace and scale’, used all too often in various management discussions In the health sector, is the antithesis of what the NHS needs right now. PCNs need time to build stronger relationships with their local communities, really listen to what their community are experiencing and build local solutions WITH their communities through co-design and co-creation. The constant onslaught of new targets, new measurement tools, new initiatives, all to be delivered by, well, yesterday, are completely counterproductive to the transition and revolution that community medicine needs to make. The current work load in General Practice is unsafe and unsustainable and is a byproduct of the consumerist attitude we have taken towards healthcare as a commodity. PCNs need time and will fail otherwise! This must be created for them.
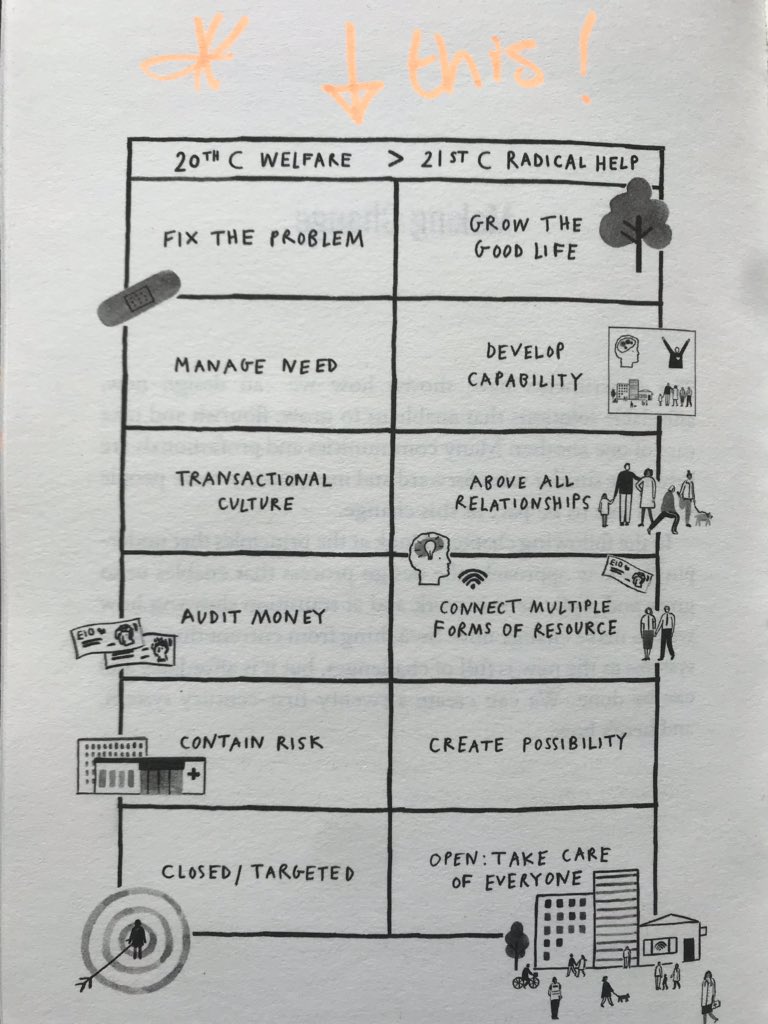
Secondly, PCNs need to look at alternative and more sustainable models for the future. Currently, PCNs are very much built around General Practice at the core, and this makes alot of sense in many ways. However, here in Morecambe Bay, we have a building block called ‘Integrated Care Communities’ (ICCs), which pre-date PCNs by some five years. I believe we need to see a melding of the best bits of both, with a much wider and more integrated team within and around the PCN model. The traditional GP partnership model, though highly successful and desirable in so many ways, continues to build a model with the GP, primarily as the leader. I am a GP Partner myself – there are some huge benefits to such a model, especially often through great altruism and genuine community care. One of the difficulties facing primary care, as it stands though, is that few ‘future GPs’ want to become partners, preferring a ‘salaried’ approach and the issues facing primary care may, perhaps require a different kind of (and perhaps more socially just) economic model. I suggest that PCNs may want to explore the highly effective and entrepreneurial model of Social Cooperatives. Such models have proved highly successful in places like The Netherlands and New Zealand, provide greater sustainability, better collaborative working and more exciting opportunities. Drawing on the work of the economists, Spencer Thompson, Kate Raworth, Mariana Mazzucato, Katherine Trebeck (and others) I can see that a social co-operative model of PCNs, given trust and freedom to experiment, by either government or commissioners, could really remodel health and care at a local level, around genuine community need, as set out by Hilary Cottam in Radical Help. We could see the creation of locally led (and owned) community health and care services (perhaps even including care homes, who are still very poorly treated as we have seen through this crisis), creating healthy communities from pre-conception to death through asset based community development and participatory, democratic processes. A social cooperative model allows all people working together in a geography to be part of the same ‘system‘, rather than the current clumsiness of multiple ‘sovereign organisations’ tripping over each other, whilst creating similar community roles, bespoke to each employer’s whim. However, a cooperative model may not work for all organisations, like the police and fire-service (I’m happy to be convinced otherwise) and so building relationships, sharing milk and working having regular check-ins and multidisciplinary team meetings will continue to be important.
The possibilities at the local level are endless. PCNs would be able to prioritise a much more proactive, preventative model of health and care, employing smaller but more relational and therefore more effective and sustainable teams, embedded in local communities. They would form fantastic partnerships with local schools, co-designing a curriculum that creates positive mental and physical health, connecting young people more into their community and environment whilst being trauma-informed and compassionate in their leadership. Midwives, health visitors, social workers, community Paediatricians and mental health practitioners could form part of the core team and all work from the same geographical space with IT systems that actually talk to each other. Community care of the elderly would be more joined up, with care of the elderly physicians leading their own care of nursing home patients, supported by specialist nurse practitioners, along with, of course the incredible 3rd sector. It might be that some consultants, e.g. Rheumatologists, Dermatologists and Psychiatrists could belong to a cohort of PCNs, even employed by them, and therefore create a greater sense of belonging to a particular set of communities and they would also be able to work with communities more proactively through workshops, group consultations and education settings. Teams could flex and grow to suit the needs of a community, with the economic model set up to enable rather than constrain the flourishing of such initiatives. The social cooperatives could also form community land trusts which could begin to tackle various wider social determinants of poor health, including issues like housing, homelessness and access to green spaces. These cooperatives could ensure a living wage and persuade local businesses to get more involved in the area of health and wellbeing and even invest in the kind of initiatives that would create work in the green sector for local people. Why shouldn’t local health communities be involved in social change, when these issues affect the health of their communities so vastly?
I see local leadership teams (what we call Integrated Care Partnerships or ICPs), made up of PCN Directors, Local Government Officials, CVFS CEOs, The Police, Fire Service and Hospital Chiefs continuing to take the role of looking at a wider Population, made up of a group of PCNs and support them in tackling health inequalities, taking a servant leadership approach to empower them to succeed as much as possible. Primarily this group would be about permissioning, enabling, encouraging, holding space for learning and development, holding true to values and using data to facilitate excellence in practice. Relationships and trust will be the core ‘operating framework’ to enable PCNs to fully flourish.
The Integrated Care System (ICS) Leaders then need to take a similar approach with each ICP in their domain, giving as much power away as possible and taking a collaborative approach across a wider geography to learn from each other and encourage best practice and through the sharing of stories and success. It’s this kind of nurturing and facilitative leadership that will enable each ICP and PCN to flourish. Hospitals will naturally become more focused on acute care, and areas, like Oncolgy, as consultants become more aligned to the PCNs with which they primarily work (obviously this does not apply to all specialities, which is why an ICS can take more of an overall look at the hospital requirements for the population it serves). The role of the national NHS England and NHS Improvement teams then becomes the servant of all, the enabler and the holder of core values. Rather than a central command and control structure, it gives itself to a love-poured out model, creating cultures of joy right through the health and care system. Yes, it sets some priorities, but does so by listening to what communities around the nation are saying. So right now that would include asking PCNs to prioritise tackling systemic and ingrained racism, health inequalities and childhood trauma, in collaboration with their communities. They will take the best of international experience and learning, share that widely and reimagine the NHS as global trend-setter for how we create deep peace and wellbeing in our communities, enabling us to become good ancestors of the future. A radical, revolutionary but entirely practical refocusing of the NHS and Care System from the bottom-up is entirely possible. There is almost no remodelling needed, simply a change in focus and culture. It requires PCNs and the communities they serve to get on an do it together, disregarding that which prevents them. If they do this, they will find that everything they need will follow them and their light will shine brightly.