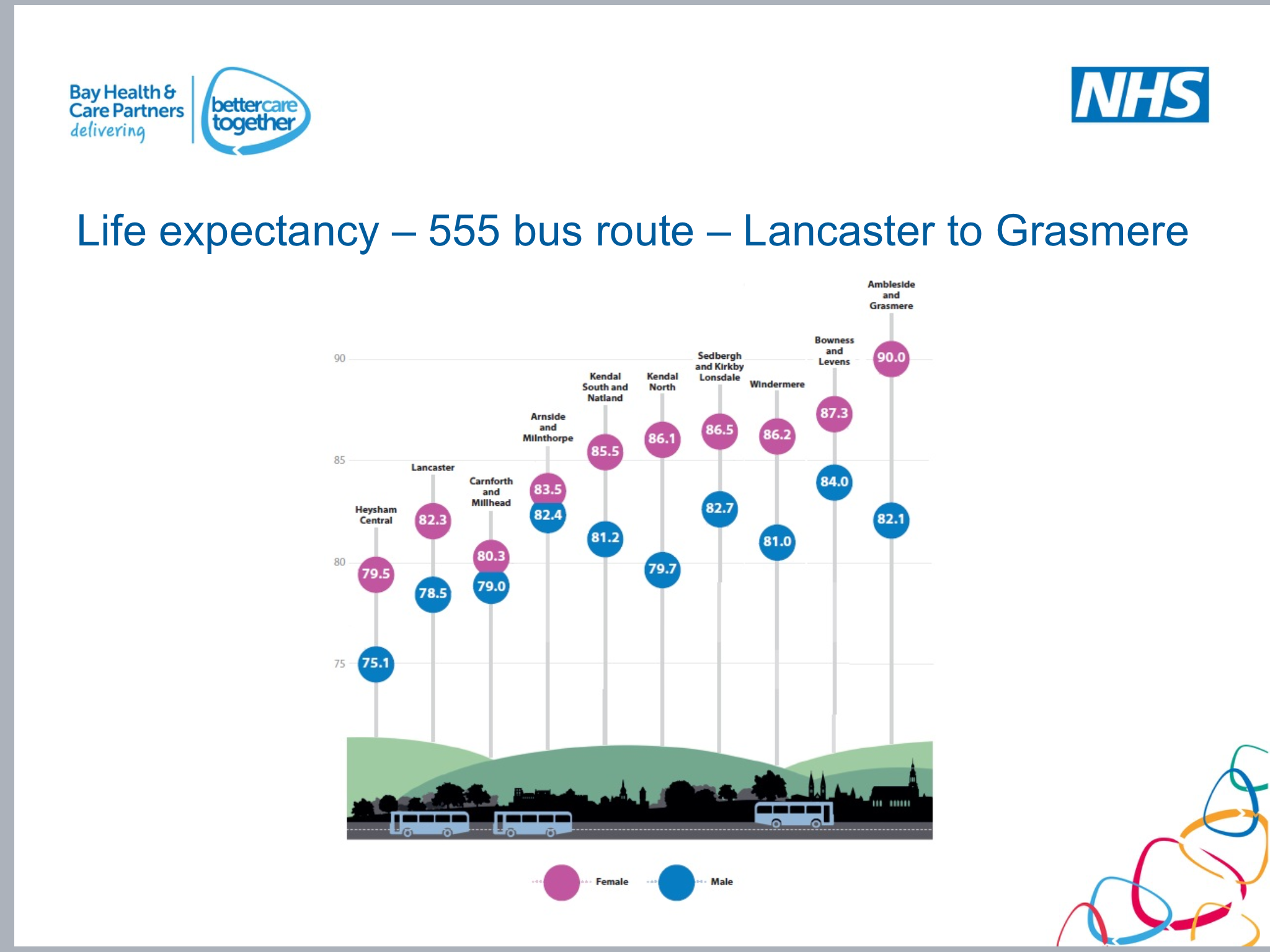
 The winter hasn’t even hit us yet. But it will and it’s going to hit us hard. Harder than we know. Harder than we are prepared for. Do you remember January 2015, with queues of people lying in corridors in our Emergency Departments, and a high spike in winter deaths? One of the people I respect most in the world of Public Health, Prof Dominic Harrison, highlighted to me this week, that it was a three-fold, intertwining cord which led to the devastating outcomes: an ineffectual flu vaccine, high staff vacancies in the NHS, and high staff sickness rates. But here’s the thing – this year we have more factors (Covid-19, incoming Influenza, staff gaps in the NHS, people having to self-isolate and sickness levels rising – this week our surgery had 14 staff off with C-19) and although, so far we haven’t seen the spike in deaths associated with the rising number of Covid-19 cases (thanks to better treatments), our hospitals are filling up fast, whilst the mantra remains, that the NHS must get back to pre-Covid levels of operation. This is going to be a tough winter. And it’s going to be worse, as it always is in our most deprived communities, which will further widen the health inequalities gap. And people are going to die, not only of Covid and influenza, but of other preventable things like heart attacks, strokes and suicide, in higher numbers than usual. What am I, a prophet of doom? Well…..I hope not! But this is a wake-up call.
The winter hasn’t even hit us yet. But it will and it’s going to hit us hard. Harder than we know. Harder than we are prepared for. Do you remember January 2015, with queues of people lying in corridors in our Emergency Departments, and a high spike in winter deaths? One of the people I respect most in the world of Public Health, Prof Dominic Harrison, highlighted to me this week, that it was a three-fold, intertwining cord which led to the devastating outcomes: an ineffectual flu vaccine, high staff vacancies in the NHS, and high staff sickness rates. But here’s the thing – this year we have more factors (Covid-19, incoming Influenza, staff gaps in the NHS, people having to self-isolate and sickness levels rising – this week our surgery had 14 staff off with C-19) and although, so far we haven’t seen the spike in deaths associated with the rising number of Covid-19 cases (thanks to better treatments), our hospitals are filling up fast, whilst the mantra remains, that the NHS must get back to pre-Covid levels of operation. This is going to be a tough winter. And it’s going to be worse, as it always is in our most deprived communities, which will further widen the health inequalities gap. And people are going to die, not only of Covid and influenza, but of other preventable things like heart attacks, strokes and suicide, in higher numbers than usual. What am I, a prophet of doom? Well…..I hope not! But this is a wake-up call.
 It’s no surprise that so many people feel a smouldering sense of anger towards the government. There is no doubt that things could and should have been handled differently from the beginning. It’s no use saying – well….we didn’t know what we were facing, we weren’t prepared for this….. the government didn’t even follow their own advice from their preparedness exercise three years ago, they have outsourced test and trace to companies with no track record or expertise in the world of public health to the tune of £12billion and it doesn’t even work effectively. They have given contradictory advice to different regions of the UK, they have continued to allow foreign travel, they have failed to adequately explain the reasons for certain policies which key members of their inner circle haven’t even followed, they have briefed key city leadership teams through the press and failed to win the public’s trust – something which is so crucial at such a time as this. They have “followed the science” and then not followed the science…..it has been a shambles and it’s no wonder that people are disengaged.
It’s no surprise that so many people feel a smouldering sense of anger towards the government. There is no doubt that things could and should have been handled differently from the beginning. It’s no use saying – well….we didn’t know what we were facing, we weren’t prepared for this….. the government didn’t even follow their own advice from their preparedness exercise three years ago, they have outsourced test and trace to companies with no track record or expertise in the world of public health to the tune of £12billion and it doesn’t even work effectively. They have given contradictory advice to different regions of the UK, they have continued to allow foreign travel, they have failed to adequately explain the reasons for certain policies which key members of their inner circle haven’t even followed, they have briefed key city leadership teams through the press and failed to win the public’s trust – something which is so crucial at such a time as this. They have “followed the science” and then not followed the science…..it has been a shambles and it’s no wonder that people are disengaged.
HOWEVER – this is not the time to let our cynicism get the better of us! What we have to face is that we are where we are and we’re heading into winter, and our anger towards these various failings is in danger of causing us to embrace apathy or rebellion – both of which will have terrible consequences. So right now, we need to keep our heads and we need to take a deep breath. There will come a time for the government to answer serious questions about how they have handled this pandemic and the decisions they have made. But it is not now. Now, we need to look ahead and be really pragmatic about what we’re about to face together.
 Firstly, I would implore the government to listen to the wisdom of Prof Devi Sridhar. As the youngest ever Rhodes Scholar and fiercely respected Professor of Global Public Health, she is worth listening to. She has not been shy in her critique of where the government have made mistakes. But she is also speaking with a real sense of pragmatism and kindness, as she draws on lessons from across the globe to develop a roadmap for the way ahead. Her advice to government is as follows:
Firstly, I would implore the government to listen to the wisdom of Prof Devi Sridhar. As the youngest ever Rhodes Scholar and fiercely respected Professor of Global Public Health, she is worth listening to. She has not been shy in her critique of where the government have made mistakes. But she is also speaking with a real sense of pragmatism and kindness, as she draws on lessons from across the globe to develop a roadmap for the way ahead. Her advice to government is as follows:
- Ensure the Test, Trace and Isolate system is robust. Test results need to be back within 24 hours, 80% of contacts must be traced and strict adherence to the 14 days isolation is vital. The current system still isn’t working effectively enough, despite an eye watering bill with no sense of accountability or responsibility for it’s failure. It is not too late to ensure that local directors of Public Health can lead this work heading into winter and ensure that all available labs are put to effective use.
- Solid, consistent and clear public health messaging needs to go to the public through every means possible. There needs to be rationale and helpful explanations about why certain measures are being chosen.
- We need strict border measures to stop the virus from re-circling.
 Secondly, as the public we need to take whatever responsibility we can to ensure we continue to do all we can. Conspiracy theories are not even vaguely helpful right now. And although it’s true that death rates have been lower than expected, there are other things to consider. This is still a dangerous virus – it will lead to many extra admissions to hospital through the winter period, especially linked with Respiratory Illness and it will affect unsuspecting and previously healthy people with the effects of long-covid – I have seen the effects of this in my (young and previously fit) patients and friends and it is truly debilitating. With all the other things we have to cope with this winter, we can’t afford to let our guard down – not now. We know from public health data that the vast majority of spread is between family, friends and neighbours. We also know that it won’t just be Covid-19 that kills people this winter. Higher than normal deaths from other illnesses/conditions are expected across the board. So, here are some sensible things we can all do to try and stay well:
Secondly, as the public we need to take whatever responsibility we can to ensure we continue to do all we can. Conspiracy theories are not even vaguely helpful right now. And although it’s true that death rates have been lower than expected, there are other things to consider. This is still a dangerous virus – it will lead to many extra admissions to hospital through the winter period, especially linked with Respiratory Illness and it will affect unsuspecting and previously healthy people with the effects of long-covid – I have seen the effects of this in my (young and previously fit) patients and friends and it is truly debilitating. With all the other things we have to cope with this winter, we can’t afford to let our guard down – not now. We know from public health data that the vast majority of spread is between family, friends and neighbours. We also know that it won’t just be Covid-19 that kills people this winter. Higher than normal deaths from other illnesses/conditions are expected across the board. So, here are some sensible things we can all do to try and stay well:
- Have a flu jab if you’re in one of the ‘at risk’ groups
- Take worrying symptoms seriously! Don’t ignore chest pain (especially if it’s worse when you exert yourself), or new lumps and bumps – especially in your more private parts, or bleeding from somewhere you don’t normally bleed from, or unexplained weight loss. See your GP!
- Wash your hands regularly
- Wear a face mask when out and about
- Spray and wipe down surfaces
- When you cough or sneeze, do so into your elbow crease
- Keep 2 metres apart from people who are not in your household, and wear a facemask if you have to get closer
- Keep within your household bubble – the vast majority of spread is now happening between family, friends and neighbours – we can’t be blazé about this!
- As far as possible (recognising that choices are significantly reduced for many of our communities), make good choices for your own physical and mental health:
- Eat well – be determined to fuel your body with good nutrients – if you’re trying to get to a more healthy weight then significantly reduce salt, alcohol, sugar and carbohydrate in your diet. Consider taking a vitamin D supplement through the winter – 1000units daily – only about £1 for 60 tablets from most pharmacies.
- Exercise – this doesn’t have to be anything unrealistic or intense – stop looking at other people’s sculptured bodies and feeling crap about yourself. You are beautiful! Just take a walk, if you’re able, every day – whatever the weather, and get some fresh air. If you’re unable to walk, try some gentle chair-based exercises – it doesn’t have to be anything heroic – something is better than nothing. Do more if you want, but let it become enjoyable, rather than a chore – something you’re choosing in order to make life better and more happy.
- Be grateful – everyday, when you wake up and before you sleep – try and think of three things you can be grateful for that day.
- Breathe deeply and use breathing techniques to calm yourself down, like box breathing (breathe in for 4, hold in for 4, breathe out for 4, hold out for 4).
- Connect with people – even if it’s via zoom, facetime or the phone – whatever it takes – connect with other human beings around you. Social isolation is literally a killer. We must take care of each other. Ask people how they are and genuinely care enough to listen. Some people are going to tell you they aren’t sure they want to carry on living. Ask them if they are thinking about ending their life. If they say yes – ask them if they have made any plans. Either way, take this seriously. Help them get help. Ask them if they have phoned their GP yet. Tell them you’re going to to keep walking with them through this tunnel. Reassure them that there is a light even though they can’t see it right now.
- Learn something new – a language, a skill, whatever you fancy – give it a go.
- Relax – seriously switch off the 24 hours news cycle, disconnect from too much social media and take time to do things which are good for your soul – sing, dance, read, play games, take long baths, whatever helps…..
- Sleep – our bodies and our minds regenerate when we sleep. Sleep is good!
- Above all – keep love and hope alive. We’ve got to dig deep to keep loving each other – being kind in our attitudes, even towards our enemies. And keep on keeping on hoping. If you’re not sure how, this podcast with Brené Brown and Michael Curry will help!
 Thirdly, the NHS is not yet ready. Yes – there have been some remarkable things which the NHS has done to respond to the first wave of Covid. Contrary to some misleading articles about General Practice, we are and have always remained open and available to our patients. We are triaging all patients via the phone to work out how we can best help and employing loads more technology to help us do this. It’s so much better for a young mum of three kids to be able to have quick video-call about one of her children’s rashes than have to lug them all down to the surgery. It’s great that we can now supplement a phone/video call with an advice sheet sent to your phone. It also means that we can prioritise who really needs seeing face to face and keep our premises as Covid-secure as possible. Many community staff were redeployed from their usual work, such as Speech and Language Therapists, Occupational Therapists and Physiotherapists, into the Nightingale and Rehabilitation hospitals, meaning they were taken away from their usual work, with a huge amount to now catch up on. This was not without cost to families who needed their support or were awaiting a diagnosis, and added to the strain in General Practice also. It was tough. But it was worth it. And we’re so grateful for the way the public were overwhelmingly understanding towards us as we tried to flex our services to cope with the demand.
Thirdly, the NHS is not yet ready. Yes – there have been some remarkable things which the NHS has done to respond to the first wave of Covid. Contrary to some misleading articles about General Practice, we are and have always remained open and available to our patients. We are triaging all patients via the phone to work out how we can best help and employing loads more technology to help us do this. It’s so much better for a young mum of three kids to be able to have quick video-call about one of her children’s rashes than have to lug them all down to the surgery. It’s great that we can now supplement a phone/video call with an advice sheet sent to your phone. It also means that we can prioritise who really needs seeing face to face and keep our premises as Covid-secure as possible. Many community staff were redeployed from their usual work, such as Speech and Language Therapists, Occupational Therapists and Physiotherapists, into the Nightingale and Rehabilitation hospitals, meaning they were taken away from their usual work, with a huge amount to now catch up on. This was not without cost to families who needed their support or were awaiting a diagnosis, and added to the strain in General Practice also. It was tough. But it was worth it. And we’re so grateful for the way the public were overwhelmingly understanding towards us as we tried to flex our services to cope with the demand.
 However, we need to take a radical stocktake of where we are and again put into motion some very different ways of operating over the next 2-4 weeks. It will allow us to work in a way that is safest for the public and will provide a sense of reassurance. Although I welcome the reopening of the Northern Nightingale Hospitals – as usual, the focus is far too much on the Acute Hospital sector and not enough on how we can help people stay more well in the community and prevent admission, particularly in our economically poorest communities. It’s important that the public understand that we need to reorganise our services in the community again in order to try and enable as many people as possible to stay well through this winter, particularly in our poorest communities, where admission to hospital and early death rates are always significantly higher.
However, we need to take a radical stocktake of where we are and again put into motion some very different ways of operating over the next 2-4 weeks. It will allow us to work in a way that is safest for the public and will provide a sense of reassurance. Although I welcome the reopening of the Northern Nightingale Hospitals – as usual, the focus is far too much on the Acute Hospital sector and not enough on how we can help people stay more well in the community and prevent admission, particularly in our economically poorest communities. It’s important that the public understand that we need to reorganise our services in the community again in order to try and enable as many people as possible to stay well through this winter, particularly in our poorest communities, where admission to hospital and early death rates are always significantly higher.
 I have nothing but compassion and camaraderie with GP colleagues as they cope with a huge surge in demand, (just indeed as I do with all NHS workers and carers right now, whatever their role). What I believe we need to do NOW though is change the way we’re working so that we can give real focus into the areas which are likely to affect people’s health most significantly over the months ahead, support our community colleagues to focus on various aspects of their work more effectively and enable our teams to be resilient and stay well themselves through the winter, whilst serving the communities with their usual brilliance. Here are my suggestions, which we are exploring in more depth across Morecambe Bay and indeed our Integrated Care System across Lancashire and South Cumbria (though important to note that this is more about function than form, so might ‘look’ different in each locality):
I have nothing but compassion and camaraderie with GP colleagues as they cope with a huge surge in demand, (just indeed as I do with all NHS workers and carers right now, whatever their role). What I believe we need to do NOW though is change the way we’re working so that we can give real focus into the areas which are likely to affect people’s health most significantly over the months ahead, support our community colleagues to focus on various aspects of their work more effectively and enable our teams to be resilient and stay well themselves through the winter, whilst serving the communities with their usual brilliance. Here are my suggestions, which we are exploring in more depth across Morecambe Bay and indeed our Integrated Care System across Lancashire and South Cumbria (though important to note that this is more about function than form, so might ‘look’ different in each locality):
- accept now that we cannot get back up to pre-covid levels of activity, for example in routinely scheduled operations, and if we try to, it will lead to more unnecessary deaths. This is a big ask for people who are waiting for their hip to be replaced, or their hernia to be repaired, but we have to be realistic about what is possible with the resources we have available.
- re-focus and align existing capacity in order to ensure a more coordinated approach to addressing demand.
- target additional resource to mobilise capacity where it will have the most impact.
- use data and evidence of risk and vulnerability from COVID-19 in a more systematic way to inform a response that is scaled appropriately.
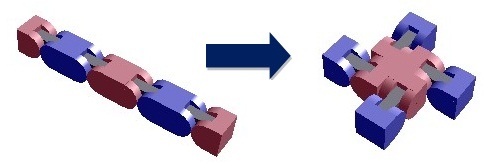
- In order for this to work practically, we must create a model which makes this possible. Perhaps one way is by reorganising into a model of Red, Amber and Green Community Hubs, supported by a co-ordination centre, which pulls together the data and brings aid when practices are struggling, could work in the following way and allow us to work as effectively as possible (recognising that this may vary according to Primary Care Network/ICP/MCP need and capability/capacity):
Red Hubs (which can be remote in terms of triage) staffed by Paramedics, GPs and Nurse Practitioners, to deal with COVID-19, Flu, and Acute Respiratory Illness (i.e. anyone with a fever, cough or breathlessness). It may be that out of hours providers may already be in place to supplement and support this model.
Amber Hubs – a remodelled care co-ordination team approach led by the General Practice Team with proactive support from community (including mental health) teams. They would use an asset based community development model of Population Health Management and work WITH communities to:
- Focus and drive on proactive long-term condition management AND other acute illnesses that don’t fit the criteria for the red hubs.
- Have a driving focus on proactive long-term condition management with particular emphasis on conditions more vulnerable to poor outcomes from COVID-19.
- Be supported by redeployed medical specialities.
- Fund and support the Community Voluntary Faith Sector to partner with Primary Care and Community Teams to create a really resilient partnership in doing this work together, recognising the HUGE impact the 3rd sector makes to this work and how fragile they are in terms of adequate resources.
- Be sited so as to ensure accessibility to residents within the 20% most deprived communities within each ICP/MCP.
- Have attached to them place based multidisciplinary assertive and active case management and care co-ordination teams (think spokes) as outlined previously. These teams would have a focus on the “priority wards” and groups experiencing higher levels of social isolation.
- Take a “more than medicine” approach by having active in reach from other partners reflecting broader, social needs that are barriers to improved health and wellbeing; social prescribing, housing, employment and more as informed by the data.
- Cardiovascular Interventions
- Hypertension – we have too many patients with a BP >150/90 (current guidance shows we should be aiming for <135/85 for the general population and <130/80 for those Diabetes or known heart disease). We will best prevent MIs and CVAs by being much more proactive in this area.
- Atrial Fibrillation – ongoing protection work by ensuring appropriate anticoagulation in those with a Cha2ds2vasc score of over 2.
- Diabetes (and Cancer)
- focus on healthy weight, driving down BMI where possible, through targeted interventions and
- reducing HbA1c in people through targeted lifestyle interventions and medication where necessary.
- Respiratory Disease (and Cancer)
- Stop Smoking interventions
- Weight loss programmes
- Winter warmth schemes in homes and damp removal – this will be vital in keeping admissions down
- Cancer – Getting a real focus on 2 week wait referrals with appropriate messaging to the public
- Mental Health – Suicide Preventions
- Mental Health reviews
- Targeted messaging to the public to help them understand why and how things are changing
- Suicide awareness training
- Frailty and Care Home work – ongoing support and focus on the frail and those in care homes
Green Hubs – these will focus on:
- Musculoskeletal problems – physio first and possible redeployment of Orthopaedic Surgeons and Pain Specialists, to run clinics and provide joint injections in the community rather than surgical procedures, to see people through the winter period
- Other day to day, essential General Practice issues – baby checks, smear tests, dermatology, rheumatology, ENT, low level mental health etc – run by a reworked and repositioned team
The model above won’t work for all, but the principles are important. It might all seem a bit radical and it’s true that there would need to be a significant amount of resource and support flowing into the community to enable this – however, if we don’t do something like this, then it’s like knowing an earthquake is coming and not bothering to take aversive action. We don’t have the personnel we need right now, but partnering with the voluntary sector (with appropriate resource allocated) and ensuring we have the right data help and support will make this more possible. Finances must be freed up to support this model and NHSE need to give the ICS teams across the nation some slack to take this more proactive approach. It will actually lead to huge savings (of lives and money).
We’ve already lost a lot of people to Covid-19. We’re heading into a serious economic catastrophe and a winter of discontent. Good public health and good health care IS good economics. If the government heed the warnings, if the public take this seriously and work with us, if the NHS can reorganise, even at this late stage, then we will significantly improve our chances of getting through this winter well together. We won’t have another opportunity to ‘get this right’. I hope we will act now and find that we really can make it through together.