Last week, I had a sixth form student spend the week with me. She is hoping to go to medical school and is gaining the necessary work experience ahead of her applications. It was so great to be able to share with her the variance of my work and the great privilege it is to be a GP in the community. On the first day, we saw people with all kinds of problems, often interlinked or overlapping. She was amazed by how well I know my patients, not just the conditions they have, but them as people and the complexities of their lives. At Ash Trees Surgery, the practice where I am a partner, we run personal lists, in which we as GPs always see the same set of patients, supported by 2 other doctors, for times when one of us is not around. It gives us the opportunity of building fantastic therapeutic relationships with the people we serve and we get to know them really well. Our patients love it, we love it, and it has been a ‘traditional model’ of General Practice in our local community.
However, things are changing (not immediately in our case, but faster than perhaps we would like), and we (as GPs) and people generally, are going to have to get used to it, not just in Carnforth, but across the whole of the UK. I’m not writing this blog post as an idealist, but as a pragmatist. There are many things I wish were not changing, but we are reaching a point at which the scales are tipping and things simply cannot remain as they have been. Many GPs know this already and are making bold and difficult decisions to try and work differently, but many of us keep harking back to yesteryear and wishing we could turn the clocks back.
The issues facing us are stark:
1) We simply will not have enough GPs within the next 5 years to carry on working in the ways we have done. 40% of current GPs will be retiring within the next 5 years or moving into other work. (http://www.telegraph.co.uk/science/2017/07/30/nearly-40-per-cent-gps-plan-leave-nhs-within-five-years/).
2) The promise of 5000 more GPs will simply not come to fruition and certainly not in the time frame needed. Actually, a plan is afoot to replace some of the GPs with ‘Physician Associates’, people who have a science or allied degree, who have then done a conversation course and can do some (but certainly not all) of the work of a GP. They will also neeed supervision by GPs. Health Education England are having to cut GP training in order to make way for this new breed of health care workers (yet unproven). The Royal College welcomes the development as a support, but not a replacement of GPs. (http://www.pulsetoday.co.uk/your-practice/practice-topics/education/gp-training-cuts-necessary-to-allow-hee-to-develop-physician-associates/20034643.article#.WUrZgli-YHU.twitter)
3) The new generation of GPs, do not want to become partners and therefore the old partnership model will soon become entirely unsustainable. The results of a recent survey, carried out by Pulse of GP Trainers about the future careers aspirations of their trainees is pretty stark:
Only 6% said their trainees wanted to go into partnerships;
49% said their trainees wanted to become locums;
28% said their trainees wanted to go abroad
30% said their trainees wanted to find a salaried post;
4% said their trainees wanted to change career.
So, in summary, the older GPs are retiring, we’re not recruiting enough new GPs and those we are recruiting, simply don’t want to work in the ways we have been used to.
The Five Year Forward View has been trying to encourage us all to reimagine General Practice and how we might hold true to the values of this bedrock of the NHS, whilst adapting towards the future that is coming. I think we have some options, and GPs need to think clearly and carefully about which direction they want to head in. But even more importantly, the people of the UK need to recognise that change is afoot and GPs are simply unable to work as we have done previously. The demand is too great and the resource simply is not there to carry on as we were.
The first option, is for GPs to bury their heads in the sand and hope that all this might not be true, to become more entrenched in their position and wait for things to be done to them. I believe this will be harmful for General Practice itself, as it will mean a decrease in resources, an increasingly burdensome workload and significant burnout. But I also believe it is detrimental to the NHS as a whole. We neeed to break down the barriers that have divided us and work more holistically across what is a very complex system. Waving the flag of traditional General Practice is admirable in some ways, but I think it might prevent us from stepping into the future that the nation now needs from its NHS.
The second option is for GPs to federate with other practices, keeping hold of some of what they love, (a perceived sense of autonomy, the ability to run their own business, to stay part of a smaller team) whilst benefiting from sharing some functions like training, recruitment and maybe some staff with other practices. We have done this in Morecambe Bay (thanks to the Stirling work of Rahul Keith, John Miles, Lauren Butler, Richard Russell, Graham Atkinson, Chris Coldwell et al). However, the federated model has to be given true commitment and financial support or it will accomplish very little. Practices cannot go back to competitive mindsets or taking care of their own needs first. It requires a bigger heart and a more open mind with genuine behavioural change.
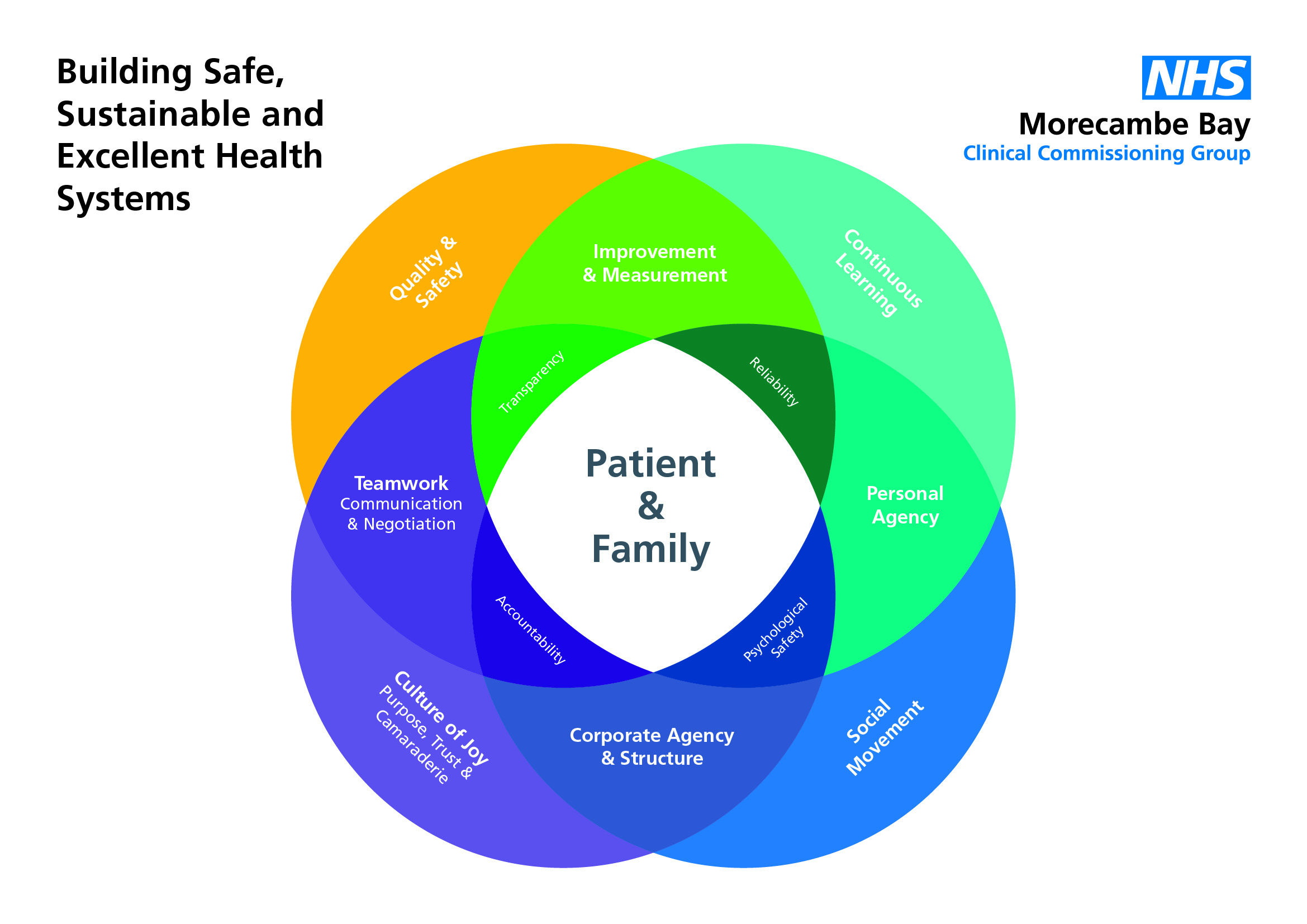
The third option is to form super-practices. We have two in our area now (Bay Medical Group in Morecambe – > 60000 patients and Lancaster Medical Practice >50000 – also both part of our federation). There are some huge advantages in working “at scale”, but it is not easy and certainly not a smooth transition. GPs have to learn to trust each other and be willing to have difficult conversations around buildings, drawings, policies etc, let alone learning to work differently. But more than that it is very hard to learn how to deliver really good General Practice in a personal way, whilst trying to reconfigure the team and establishing a really good culture. However, this model definitely allows new ways of working to be more easily acheivable, if given appropriate OD support. Some recent work done in Gosport and showcased by the King’s Fund showed that perhaps only 9% of people who phone asking to see a GP actually need to see a GP. The reality is that people have become used to seeing their GP, but often they could be seen and treated more effectively by a pharmacist, a nurse, a nurse practitioner, a physiotherapist, a mental health worker, a physician associate or a health coach. Perhaps GPs need to let go, whilst patients learn to trust the expertise of others? How do we transition to this kind of approach without losing that amazing knowledge of a community and complex social dynamics, often held by a GP? How does a Multi-Disciplinary team function effectively for the best care possible for patients in such a dynamic? We are in danger of losing something very precious, but can we somehow hold onto it in a different way?
The fourth option is to allow a “take-over” and become a more active player in an Accountable Care Organisation. The take-over approach is not straightforward, but I’m not sure it is as terrible as it appears to many GP colleagues. What if an acute trust set up a separate company, lead by a GP as medical director, who understood and held the true values of General Practice in his/her heart (as they have done in Yeovil – https://www.england.nhs.uk/blog/paul-mears-berge-balian/)? The company, run by General Practitioners, holding true to the core delivery of General Practice, without all the difficulties of running a business, HR issues, estates, etc etc but with all the benefits of shared IT systems, easier access to scans, no duplication of work and direct access to services without all the current clunkiness, not to mention protected admin time! What if the salary was right and the dross was removed? What is it exactly that would not be appealing about this? It is interesting to me. Only a couple of years ago I would have been utterly opposed to this idea, but having given it thought and time over several months, exploring the possibilities involved, I’m in the place of thinking that the benefits probably outweigh the negatives both for GPs and our patients.
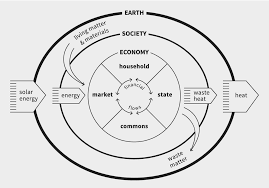
What we need right now is for us all to accept that the NHS, as we have known it is no longer functioning in a way that meets the need of the population we seek to serve. We know we need a greater emphasis on prevention and population health (I have blogged on this many times before and will do so again!). We also know that the system itself is vastly complex and is in need of major reform and reconfiguration. We need this not only for the people who use the NHS, but for those of us who work in it and are in danger of serious burn out. I hope with all my heart that General Practice does not drag its feet and prevent the revolution that is needed. Our case for more resource and more recognition of the fabulous work we do will only gain favour, if we also show that we are willing to be a part of the whole and a part of the change that must ensue.