Here is the 4th vlog in a mini-series, exploring the 5 ways to well-being from the New Economics Foundation to help transform the culture of the NHS.
Here is the 4th vlog in a mini-series, exploring the 5 ways to well-being from the New Economics Foundation to help transform the culture of the NHS.
We live in a political climate in which it appears that those in power do not listen to the voices of the ‘multitude’ (e.g. with the current protests around the NHS and education), but press ahead with their own agendas regardless. This is not only true of the current government, but a symptom of the way in which our entire political systems are set up. Here in Morecambe Bay, we need to recover the power of people movements and decide together what kind of future we want. Here is an invitation to come and be part of the emerging conversations about health, well-being and the health system around the Bay.
One of the hats I wear is to be the Clinical Lead Commissioner for Maternity Services in North Lancashire and I chair the Maternity Commissioning Group for Morecambe Bay.  Over the last few years, Morecambe Bay has been under huge public and governmental scrutiny due to some sad and significant failings at UHMBFT, our acute NHS Trust. This lead to the in-depth and wide-ranging “Kirkup Review” through which we have learned together some sobering and important lessons.
Over the last few years, Morecambe Bay has been under huge public and governmental scrutiny due to some sad and significant failings at UHMBFT, our acute NHS Trust. This lead to the in-depth and wide-ranging “Kirkup Review” through which we have learned together some sobering and important lessons.
In 2013, we carried out what is called a ‘Picker Survey’ in the Bay and had a startling reality check. 44% of the women we aimed to care for told us that they did not feel treated with kindness or respect. It was a devastating figure for us to hear. So, learning from the ‘Leeds Poverty Truth Challenge’, we learned that we needed to allow ourselves to really listen to what women were saying to us, to hear their stories and let the impact of those stories begin to change us. One of the great advocates for women, compassionate care, kind listening and careful communication in this area is Mel Gard, a Doula, who facilitates our ‘Maternity Services Liaison Committee’ (MSLC) around the Bay. The MSLC is a group of women and men who use our services, which Julia Westaway must be credited for facilitating so well. Over the last three years in particular, they have taken the time to build relationships with those of us who commission and provide services and in effect ‘speak truth to power’. Mel and many others have brought to us stories of times when listening and communication skills have been excellent within our maternity service and times when they have been clumsy at best and detrimental or abusive at worst. This has begun a culture change and a survey carried out in 2015 has seen this startling figure reduce to 26% (we know this is still far too high, but it is a vast improvement).
commission and provide services and in effect ‘speak truth to power’. Mel and many others have brought to us stories of times when listening and communication skills have been excellent within our maternity service and times when they have been clumsy at best and detrimental or abusive at worst. This has begun a culture change and a survey carried out in 2015 has seen this startling figure reduce to 26% (we know this is still far too high, but it is a vast improvement).
It is only in encountering the ‘other’ that we are really changed. Alan Alda says this, “Listening is being able to be changed by the other person.” There is no point in hearing the stories and impact of poor communication on our patients if it does not fundamentally change us and our practice. In the NHS, we’re so used to being the experts that we sometimes think we have the right to tell people what they should do, rather than really listening to them and understanding what is important to them, the person who is the expert in their own life and situation. It is partnership and not dictatorship that we need. It is a willingness to learn together rather than an arrogance that knows how to ‘fix’ things that we must develop. So, together with the MSLC we have devised an entire learning exercise for all those who work within our maternity service. We are going to allow ourselves to encounter the ‘other’, on their terms, not ours, and let the impact of their stories transform us. So, in the next couple of weeks, women from around the Bay are going to film and tell their stories in a variety of ways and this film will then be used as a learning tool for every person who works in our service around the Bay, including cleaners, the nursing auxiliary team, midwives, obstetricians of all grades etc in some wide-ranging attitudinal and communication training. Amazingly, we have just won a national grant of £65000 to help us do this really well, thanks to the exceptional work of Lindsay Lewis, our lead manager and Sascha Wells, our Head of Midwifery.
 The idea is straight forward. By hearing the real life stories from around the Bay and allowing ourselves to be impacted by them, we will then use some reflective conversations, and techniques from the ‘Art of Hosting’, to allow the power of real listening to change us and transform our practices. I am so grateful for the women and men who have been brave enough to tell their stories. I am grateful to our senior team that we have b
The idea is straight forward. By hearing the real life stories from around the Bay and allowing ourselves to be impacted by them, we will then use some reflective conversations, and techniques from the ‘Art of Hosting’, to allow the power of real listening to change us and transform our practices. I am so grateful for the women and men who have been brave enough to tell their stories. I am grateful to our senior team that we have b een willing to be humble and be impacted by these stories. I am grateful for relationships and partnerships that are being established between those of us who provide services and those who use them. I am grateful for the tenacity of people who want to see our cultures change. I am grateful for ‘The Leeds Poverty Truth Challenge’ and its far reaching consequences. I am grateful for the opportunity to break down barriers and find positive ways forward. I am grateful for the transformative power of listening and the change that can happen when we really encounter another human being. Better Care Together is so much better when we work together with those we are trying to serve.
een willing to be humble and be impacted by these stories. I am grateful for relationships and partnerships that are being established between those of us who provide services and those who use them. I am grateful for the tenacity of people who want to see our cultures change. I am grateful for ‘The Leeds Poverty Truth Challenge’ and its far reaching consequences. I am grateful for the opportunity to break down barriers and find positive ways forward. I am grateful for the transformative power of listening and the change that can happen when we really encounter another human being. Better Care Together is so much better when we work together with those we are trying to serve.
Stanley Hauerwas said this: “I was smart, but I had not yet learned to listen.” The NHS is full of really smart people. When we learn to listen, our ‘smartness’ will become real wisdom, and with wisdom, we can bring real, lasting change.
 Better Care Together is the way in which health services are now being redesigned and reorganised around Morecambe Bay, so that we can provide the best care we can for the people who live here in a way that is safe, sustainable and accessible. It is an on-going process and involves the breaking down of barriers between General Practices, the Hospital Trust (UHMBT), Community Nursing and Therapies, Mental Health Services, Social Care, Allied Services – like the Police and Fire Service – and the Voluntary Sector.
Better Care Together is the way in which health services are now being redesigned and reorganised around Morecambe Bay, so that we can provide the best care we can for the people who live here in a way that is safe, sustainable and accessible. It is an on-going process and involves the breaking down of barriers between General Practices, the Hospital Trust (UHMBT), Community Nursing and Therapies, Mental Health Services, Social Care, Allied Services – like the Police and Fire Service – and the Voluntary Sector.
Here in Carnforth, we are piloting some work around ‘self-care’ and exploring what it means to be a healthy town. This is now beginning to spread like wild fire around this area, which is exciting to watch! Part of this work is rooted in the fact that currently 1 in every 5 pounds spent in the NHS is due to our lifestyle choices. If we’re going to have a NHS in the future, then we need to try and choose to live more healthily together. We must also recognise that being healthy and well is far more than just physical health. It includes mental health, social heath and systemic (or environmental) health. A few months ago we hosted a number of conversations in Carnforth about what it might be like if Carnforth was the healthiest town in Lancashire. Some really interesting ideas emerged from the community about singing together more regularly, having less dog poo on the streets, creating safe places for the children to play, getting more exercise into our schools, encouraging healthy eating, a mental health café, help for carers and many other brilliant suggestions.
From these conversations, a ‘Self Care Tree’ has grown with four roots and three clear branches that we believe will help us grow together into a healthy and well town. The roots are straight forward –![tn_TreeRoots_resized_b-300x300[1]](http://reimagininghealth.com/wp-content/uploads/2016/03/tn_TreeRoots_resized_b-300x3001.jpg) 1) Really learning to engage with our local community instead of assuming that we know what they need and learning to do things with them instead of to them, 2) being part of an Integrated Care Community – see below, 3) Being part of Better Care Together, 4) Understanding Wellbeing – shifting our mindsets from an ‘illness model’ of health to a ‘wellness model’.
1) Really learning to engage with our local community instead of assuming that we know what they need and learning to do things with them instead of to them, 2) being part of an Integrated Care Community – see below, 3) Being part of Better Care Together, 4) Understanding Wellbeing – shifting our mindsets from an ‘illness model’ of health to a ‘wellness model’.
The three main branches we have developed in Carnforth are as follows: The first is that we have some ‘culture change’ to undergo, both in our medical and nursing teams and also as a wider community. Over the coming months we will see the emergence of what we are calling an Integrated Care Community – first modelled for this area in Garstang. As part of Better Care Together, we have appointed a fantastic new Care Co-ordinator, Sarah Baines, who was part of our District Nursing team. Sarah will work alongside Dr David Wrigley at Ash Trees Surgery to help co-ordinate care more effectively in the community for people with more complex health problems and provide more stream-lined care, preventing unnecessary hospital admissions and enabling faster and smoother discharges back home from hospital. Secondly, we are learning to take more of a ‘coaching’ approach to how we consult with patients, to encourage more partnership working with people, rather than telling people what to do (which isn’t actually very effective). Staff are training in ‘coaching practice’, ‘motivational interviewing’ and ‘shared decision making’. We are trying to be more proactive with information. If you look on our practice website, www.ashtrees.co.uk, you will find a tab entitled ‘self-care’. Here you will find videos (many more to come and some of which we are re-doing!) that talk about various common conditions you can treat yourself without having to go through the often difficult task of finding an appointment with one of our team. Our local pharmacists are a hugely valuable resource, who can offer excellent health advice and treatments over the counter, saving local people time and inconvenience. Also, not too far away, we hope to have a brilliant new facility called ‘e-consult’, which will allow our patients to manage their own care more efficiently ‘on-line’.
![Stack-of-British-one-pound-coins-1516897[1]](http://reimagininghealth.com/wp-content/uploads/2016/03/Stack-of-British-one-pound-coins-15168971.jpg) The pressure on General Practice is huge. The government only allocates £136 per person per year to General Practice. this money accounts for all GP consultations, appointments with nurses, blood tests, investigations and referrals and indeed the payment of staff. If you want to know what this compares to, then for £136, you can buy 11 months worth of pet insurance for a rabbit or 3 months worth of coffee every day on your way to work!! No wonder the system is under strain! If we want to have a NHS that is free for everybody and still standing in the years ahead for future generations, then we do need to be careful that we don’t abuse the system and take care of ourselves better and think about whether we really need an appointment before booking one!
The pressure on General Practice is huge. The government only allocates £136 per person per year to General Practice. this money accounts for all GP consultations, appointments with nurses, blood tests, investigations and referrals and indeed the payment of staff. If you want to know what this compares to, then for £136, you can buy 11 months worth of pet insurance for a rabbit or 3 months worth of coffee every day on your way to work!! No wonder the system is under strain! If we want to have a NHS that is free for everybody and still standing in the years ahead for future generations, then we do need to be careful that we don’t abuse the system and take care of ourselves better and think about whether we really need an appointment before booking one!
The second branch we have seen is the emergence of ‘community leaders’, who have seen a community need and have stood up to do something about it. We know there are already loads of ![il_340x270.575369125_lhd6[1]](http://reimagininghealth.com/wp-content/uploads/2016/03/il_340x270.575369125_lhd61.jpg) community leaders out there doing great stuff, like sports clubs as just one example. So, we have seen the start of a mental health café, called “Serenity” every Wednesday afternoon at Hunter Street in Carnforth, 2-4pm. A carer’s café has started on the 3rd Saturday of every month 2-4pm, again at Hunter Street. Carnforth Community Choir meets at 7pm every Friday evening at the Civic Hall – singing is well known to improve our health and wellbeing! We have volunteer dog poo wardens, trying to help our streets be cleaner (it’s amazing what dog poo says about a town), and people cleaning up our parks to give the children in our community safe places to play outdoors. We have trained 22 “health champions” who will be starting with various initiatives soon, and many others have volunteered to help in lots of exciting new ways. All of this serves to break down social isolation and encourage us to take care of ourselves and one another.
community leaders out there doing great stuff, like sports clubs as just one example. So, we have seen the start of a mental health café, called “Serenity” every Wednesday afternoon at Hunter Street in Carnforth, 2-4pm. A carer’s café has started on the 3rd Saturday of every month 2-4pm, again at Hunter Street. Carnforth Community Choir meets at 7pm every Friday evening at the Civic Hall – singing is well known to improve our health and wellbeing! We have volunteer dog poo wardens, trying to help our streets be cleaner (it’s amazing what dog poo says about a town), and people cleaning up our parks to give the children in our community safe places to play outdoors. We have trained 22 “health champions” who will be starting with various initiatives soon, and many others have volunteered to help in lots of exciting new ways. All of this serves to break down social isolation and encourage us to take care of ourselves and one another.
The third branch is ‘clinical leadership’. Right now, Morecambe Bay has some of the worst health outcomes in the country. We have terrible heart disease rates and people die here far too young![image[1]](http://reimagininghealth.com/wp-content/uploads/2016/03/image1.jpg) of preventable illnesses. It would be wrong of us, as clinical leaders in the community, to stand by and let these statistics continue as they are. Morecambe Bay deserves better. So, we are working with schools to encourage more exercise in the children and young people in our community. Two local schools (‘Our Lady of Lourdes, Carnforth’ and ‘Arch Bishop Hutton, Warton’, with ‘St John’s C of E, Silverdale’ soon to follow) have started running a mile a day – all children and staff! This is an amazing achievement and there are some wonderful stories emerging already of the great impact this is having on pupils and staff alike. We’re seeing huge improvements in sleep cycles, behaviour, concentration and general health. Under the banner of ‘Let’s Get Moving’ we hope that all the primary schools in the district will soon be participating in other similar initiatives. We have also started a couple of programmes of work with Carnforth High School, in line with needs they have highlighted to us. We are also going to trial a new NHS shopping list and menu to try and encourage us as a community to eat more healthily and avoid some of the unhealthy ‘bargains’ that the advertising giants try and tempt us with, cutting down on meat, alcohol, sugar and too much fat. If we don’t learn to manage our appetites and our spending habits better, we will never overcome the alarming rise in diabetes rates and heart disease. We are responsible together and really can make a change! So, not long from now, people in this area won’t even need to stress about what to cook for the week ahead, because they will be able to turn up to their local supermarket and get some really healthy and tasty ideas, all costed out and easily affordable (with huge thanks to our amazing chefs, Andy Bickle and Lee Till, from our hospital trust, working with us)! By eating more healthily and taking more exercise, we can genuinely change the health and wellbeing in this area for the next 50 years! On a different tack, our district nursing team is also beginning a leg-ulcer café for those who have been housebound. Such cafés have been proven elsewhere to break social isolation and improve healing rates for patients. All of this work is being undergirded by amazing research projects with the University of Lancaster.
of preventable illnesses. It would be wrong of us, as clinical leaders in the community, to stand by and let these statistics continue as they are. Morecambe Bay deserves better. So, we are working with schools to encourage more exercise in the children and young people in our community. Two local schools (‘Our Lady of Lourdes, Carnforth’ and ‘Arch Bishop Hutton, Warton’, with ‘St John’s C of E, Silverdale’ soon to follow) have started running a mile a day – all children and staff! This is an amazing achievement and there are some wonderful stories emerging already of the great impact this is having on pupils and staff alike. We’re seeing huge improvements in sleep cycles, behaviour, concentration and general health. Under the banner of ‘Let’s Get Moving’ we hope that all the primary schools in the district will soon be participating in other similar initiatives. We have also started a couple of programmes of work with Carnforth High School, in line with needs they have highlighted to us. We are also going to trial a new NHS shopping list and menu to try and encourage us as a community to eat more healthily and avoid some of the unhealthy ‘bargains’ that the advertising giants try and tempt us with, cutting down on meat, alcohol, sugar and too much fat. If we don’t learn to manage our appetites and our spending habits better, we will never overcome the alarming rise in diabetes rates and heart disease. We are responsible together and really can make a change! So, not long from now, people in this area won’t even need to stress about what to cook for the week ahead, because they will be able to turn up to their local supermarket and get some really healthy and tasty ideas, all costed out and easily affordable (with huge thanks to our amazing chefs, Andy Bickle and Lee Till, from our hospital trust, working with us)! By eating more healthily and taking more exercise, we can genuinely change the health and wellbeing in this area for the next 50 years! On a different tack, our district nursing team is also beginning a leg-ulcer café for those who have been housebound. Such cafés have been proven elsewhere to break social isolation and improve healing rates for patients. All of this work is being undergirded by amazing research projects with the University of Lancaster.
As part of our on-going conversation with this community, we are hosting a further ![781-T[2]](http://reimagininghealth.com/wp-content/uploads/2016/03/781-T2.jpg) evening, alongside our Mayor, Malcolm Watkins. It will be on Wednesday 6th April, 7pm at Carnforth Civic Hall. There will be other conversations in the next couple of months in Warton (for those living in Warton and Silverdale) and in Bolton-Le-Sands, for those in BLS, Halton and the Kellets. On Saturday 25th June 2016, we will also co-host a huge Health Mela at Carnforth High School. If you live in the area, please do come along to either of these events and talk with us about what is already going on and how we can all work together to make this town and district a truly healthy place.
evening, alongside our Mayor, Malcolm Watkins. It will be on Wednesday 6th April, 7pm at Carnforth Civic Hall. There will be other conversations in the next couple of months in Warton (for those living in Warton and Silverdale) and in Bolton-Le-Sands, for those in BLS, Halton and the Kellets. On Saturday 25th June 2016, we will also co-host a huge Health Mela at Carnforth High School. If you live in the area, please do come along to either of these events and talk with us about what is already going on and how we can all work together to make this town and district a truly healthy place.
 Amidst the current ‘efficiency savings’, or cuts by any other name, in the NHS, the voluntary or 3rd sector, including the faith communities are an absolutely vital partner in health and social care. Here in Morecambe Bay, we are seeing incredible work done by this sector. Genuinely, the safety net created across this Bay for people with significant mental health issues, chronic physical health complaints, those at the end of life, the isolated and lonely etc is amazing. However, as the financial squeeze increases on the NHS, the 3rd sector, although phenomenally resilient and full of social entrepreneurs with good heart, is really beginning to struggle to secure funding. If the 3rd sector, (which gives far more for far less) begins to crumble, then we will see health and social care completely collapse.
Amidst the current ‘efficiency savings’, or cuts by any other name, in the NHS, the voluntary or 3rd sector, including the faith communities are an absolutely vital partner in health and social care. Here in Morecambe Bay, we are seeing incredible work done by this sector. Genuinely, the safety net created across this Bay for people with significant mental health issues, chronic physical health complaints, those at the end of life, the isolated and lonely etc is amazing. However, as the financial squeeze increases on the NHS, the 3rd sector, although phenomenally resilient and full of social entrepreneurs with good heart, is really beginning to struggle to secure funding. If the 3rd sector, (which gives far more for far less) begins to crumble, then we will see health and social care completely collapse.
I wish truth and solutions were all black and white, but there is complex grey for us to wade through, if we are to see a more resilient 3rd sector emerge for the sake of our communities. The relationship between the NHS and 3rd sector is complex but vital. I want to briefly highlight some of the main issues and then look at two possible solutions.
So, where might some solutions lie? I would like to suggest two broad possible solutions. I admit they are not perfect and they certainly won’t be the only solutions.
![]() Firstly, here in Morecambe Bay, we are developing ICCs (Integrated Care Communities). These are built around General Practice (be that one or many practices in a geographical area) but incorporate GPs, District Nurses, Community Matrons, Long Term Condition Teams, Community Therapists, Mental Health Teams, Social Care, the City Council, the Po
Firstly, here in Morecambe Bay, we are developing ICCs (Integrated Care Communities). These are built around General Practice (be that one or many practices in a geographical area) but incorporate GPs, District Nurses, Community Matrons, Long Term Condition Teams, Community Therapists, Mental Health Teams, Social Care, the City Council, the Po lice, the Fire Service and the Third Sector all partnering together for more effective working and therefore better care for all. One option would be for each ICC to have a capitated budget which would allow each team to decide which voluntary sector organisations would meet the need of their particular areas most effectively and fund them accordingly and fairly.
lice, the Fire Service and the Third Sector all partnering together for more effective working and therefore better care for all. One option would be for each ICC to have a capitated budget which would allow each team to decide which voluntary sector organisations would meet the need of their particular areas most effectively and fund them accordingly and fairly.
 A second solution could be for the 3rd Sector to form one or several larger co-operatives. The huge advantage here is that it would then allow a more straight forward commissioning relationship and would allow the many to be become stronger and more resilient together. In a co-operative model, it would be easier to build research partnerships and accountability between members. It would also give the sector more clout as a partner round the table with the various public sector organisations.
A second solution could be for the 3rd Sector to form one or several larger co-operatives. The huge advantage here is that it would then allow a more straight forward commissioning relationship and would allow the many to be become stronger and more resilient together. In a co-operative model, it would be easier to build research partnerships and accountability between members. It would also give the sector more clout as a partner round the table with the various public sector organisations.
My work has taught me how vital the Voluntary and Faith sector is to the ongoing health and social care of our communities. It needs adequate funding and support, without which it will crumble. We need to help partner together to make it more resilient, but in order for this to happen, the 3rd sector must deal with some of it’s default towards self-protectionism and find creative solutions towards a more sustainable future……
 In all the places I have seen an ability to try something radical and new in the sphere of health and social care (Valencia and Arkansas being two prime examples), I have witnessed one key component. They have fixed the IT! It is really not beyond the wit of man, though I accept it is not altogether straightforward. However without it, change is painfully slow and it is extremely difficult to make the kind of changes we need to see. I do not understand why the Government will not invest in this area appropriately. Here in Morecambe Bay we need to crack this nut if we’re going to be able to let go of our past and embrace a truly collaborative and integrated way of working.
In all the places I have seen an ability to try something radical and new in the sphere of health and social care (Valencia and Arkansas being two prime examples), I have witnessed one key component. They have fixed the IT! It is really not beyond the wit of man, though I accept it is not altogether straightforward. However without it, change is painfully slow and it is extremely difficult to make the kind of changes we need to see. I do not understand why the Government will not invest in this area appropriately. Here in Morecambe Bay we need to crack this nut if we’re going to be able to let go of our past and embrace a truly collaborative and integrated way of working.
The benefits to everybody would be huge. Patients would have safer, more streamlined and ultimately more affordable care. This would cut the complaint and litigation culture to an absolute minimum. Clinicians would be able to work far more collaboratively, effectively, safely and efficiently. If we allow ourselves to imagine just what a difference it could make then we will act to make this a reality.
There have been some great strides forward made here by the excellent work of GPs like Tim Reynard and George Dingle, who are developing some fantastic new ways of working and building relationships between primary and secondary care. But their efforts are being hampered by a lack of a truly integrated system.
As just one example, take the referral process. If a patient comes to me asking for a referral, which may also require some complex tests to help reach a diagnosis, currently there is so much wasted time and effort plus duplication of work that it is an absolute farce. Say someone comes to see me with a suspected rheumatological condition. Currently, I can see them, assess them, order some (but not all tests) and then refer them. My notes will be on my computer system, but my letter to the consultant may not fully convey all the intricacies of the history I have taken over weeks. My letter has to be written and sent off (on occasion they get lost in the system, causing huge frustration to the patient). Then the consultant sees them……..she will probably order further tests, which she will then write to me to organise, or have them done at the hospital, then she will see the patient again. She will then start some treatment, but will write to me to prescribe it and then the patient will then come to collect it from my surgery. She also asks me to refer onto our community physio teams (a letter I read at 7pm after 11 hours of non-stop work, when I want to get home for my kids’ bedtime stories). There are several points of frustration for everybody involved in the process, not least the patient with wasted time and resources along the way (plus extra letters to answer complaints for missed referrals or whatever else might go wrong).
In an integrated system, the patient sees me. I write good and detailed notes, which I link to the consultant rheumatologist, assigned to work alongside my practice,  with a short note attached. She then liaises with me in a straightforward way about the case, decides what extra tests are required and these are organised (within appropriate resource allocation) ahead of the consultation. The consultant sees the patient, with a full history and set of investigations. She agrees a treatment course with the patient, prescribes the necessary drugs, which automatically appear in the electronic record, so my team can print out the prescription and the patient can pick it up. She also simultaneously links her consultation to the community physio with a short note and her therapy can be arranged in a slick and easy fashion. This has saved loads of steps, time, energy, complexity and errors. It is a basic example. There are many more areas, like maternity care, patients with complex medical problems involving the care of multiple departments etc where this is simply a no brainer.
with a short note attached. She then liaises with me in a straightforward way about the case, decides what extra tests are required and these are organised (within appropriate resource allocation) ahead of the consultation. The consultant sees the patient, with a full history and set of investigations. She agrees a treatment course with the patient, prescribes the necessary drugs, which automatically appear in the electronic record, so my team can print out the prescription and the patient can pick it up. She also simultaneously links her consultation to the community physio with a short note and her therapy can be arranged in a slick and easy fashion. This has saved loads of steps, time, energy, complexity and errors. It is a basic example. There are many more areas, like maternity care, patients with complex medical problems involving the care of multiple departments etc where this is simply a no brainer.
So what is stopping us? Actually it’s pretty straight forward. 1) A lack of sensible and adequate resourcing from the government within the Vanguard system, which would allow us to make significant changes in a small amount of time. Instead of concentrating on a few Vanguard sites and allowing us to really flourish, things have become far too watered down across way too many experimental initiatives and the funding promised has not been made available. This really needs to be rectified. I’m sure there are things we could also streamline within our Accountable Care System. 2) Stupid competition laws and sweeteners offered to some of our partner providers to use certain IT systems which are clunky and unfriendly when it comes to creating platforms that can talk to each other, have slowed us down. We need a focused and joined-up approach. 3) Priorities. My argument is that without integrating the IT fully and investing in front end smart IT that promotes self care and more appropriate use of resources, we will not achieve together what we could in a way that will benefit everybody.
In short, we need to fix the IT. It is the solution to a vast majority of our problems and will allow us to really have Better Care Together.
 My last post, “Time to Face The Music” was deliberately provocative. We cannot simply keep on doing what we’ve always done or nostalgically hold onto the ‘good old days’. As previously stated, it simply isn’t sustainable and we’re only deceiving ourselves if we think it is.
My last post, “Time to Face The Music” was deliberately provocative. We cannot simply keep on doing what we’ve always done or nostalgically hold onto the ‘good old days’. As previously stated, it simply isn’t sustainable and we’re only deceiving ourselves if we think it is.
We find ourselves in a a different (post flood) landscape, a terrain that requires a new way of being together. And we are fast learning, here in Morecambe Bay, that it’s not just enough to break down the traditional barriers between Hospitals, GPs, Mental Health, Community Nursing, the Emergency Services and Social Services. No, we have to go much wider and deeper than that if we’re going to develop a radically new way of working that is sustainable. We need to develop a Wellness Service that is of high quality, able to continually improve and offer compassionate, excellent, affordable, safe and accessible health and social care to everyone in our community. In order to do so, we need every person in every community to partner with us. We need partnerships with education, business, sport, justice, housing and the voluntary sector to name just a few. Old silos must be broken down and centrally driven targets must be re-examined to give communities the ability to creatively flourish together.
We need big conversations across the sectors of society about what it really means for us to be well and how we can take better responsibility for ourselves and each other. It is so much more than just physical and mental health. It must include a wider understanding of social and systemic health also (see earlier posts on this).
And this is exactly what our team in Morecambe Bay is trying to do. We’re not always getting it right and we’re learning some really tough lessons along the way, especially that our old habits of trying to fix things die hard! Real engagement takes time, but in the process of doing so, we are seeing 3 core principles emerging out of our focused work in Carnforth that we believe to be important keys to unlock this process in every community.
We’re not always getting it right and we’re learning some really tough lessons along the way, especially that our old habits of trying to fix things die hard! Real engagement takes time, but in the process of doing so, we are seeing 3 core principles emerging out of our focused work in Carnforth that we believe to be important keys to unlock this process in every community.
As we listen and engage with local people and communities, firstly we are seeing community leaders naturally rise up to make a difference and help increase the well-being of their area. We have many varied examples of amazing initiatives beginning. Secondly, we are seeing clinical leadership that is evidenced based and responsible, but empowers others to make a change. Thirdly we are seeing culture change beginning to emerge, with a more effective coaching culture and a focus on the wellness of those who deliver the care within our communities.
 Conversations really matter and carry within them the dynamic potential to make significant and lasting change, as we learn not only to talk differently, but to act differently as well. In the NHS, we have some expertise, but the true experts of their own lives and communities are the citizens we serve. We must change to be much more in conversation with them rather and lose the role of ‘grandma knows best’!
Conversations really matter and carry within them the dynamic potential to make significant and lasting change, as we learn not only to talk differently, but to act differently as well. In the NHS, we have some expertise, but the true experts of their own lives and communities are the citizens we serve. We must change to be much more in conversation with them rather and lose the role of ‘grandma knows best’!
Here is the first of a series of little video blogs about how we can change the culture of the NHS. The first cohort look at using the “5 Ways to Wellbeing” from the New Economics Forum to help us on our way. This vlog also gives a bit of an intro into the series, so is a little bit longer than the others which will follow.
 There is an ancient proverb that says: without vision, people perish. I believe we in danger of watching the NHS perish in front of our eyes, not because we don’t know what to do or even how to do it. I believe we have been so focused on the what and how of healthcare, that we may have forgotten why we do what we do.
There is an ancient proverb that says: without vision, people perish. I believe we in danger of watching the NHS perish in front of our eyes, not because we don’t know what to do or even how to do it. I believe we have been so focused on the what and how of healthcare, that we may have forgotten why we do what we do.
The NHS is an organism, made up of many living cells, called human beings, who have a vast range of complementary skills and interpersonal connectivity. These cells work  together in tissues, joined to each other in complex systems to function as a body, a body which gives itself for the health and well-being of the nation. This body is not a robot, who’s performance can be processed like a machine for a predetermined output, but it has been treated as such, just another example of biopower, where people are used, rather than cherished. So now we have more of a Tin Man with no heart, than a living, breathing body.
together in tissues, joined to each other in complex systems to function as a body, a body which gives itself for the health and well-being of the nation. This body is not a robot, who’s performance can be processed like a machine for a predetermined output, but it has been treated as such, just another example of biopower, where people are used, rather than cherished. So now we have more of a Tin Man with no heart, than a living, breathing body.
But at the heart of the NHS is what we find in the heart of every human being, if we dig deep enough. The heart of the NHS, the very core of its being, it’s true raison d’être, it’s driving force is in fact, love. And the people, the cells who work in this loving  organism, also carry love in their hearts for other people. It is stamped through the DNA. It is the motivation. It is the reason people get out of bed in the morning, or work through their weekends and nights. It is why the wards are clean and the beds are made, why the bloods are taken, the investigations are done, the research is carried out, the people are washed and fed. It is why the hours of study and audit are diligently pursued, it is why the training is so robust, it is why the skills are acquired, it is why the time is given. It is why the NHS was founded in the first place, because all people, no matter how rich or poor, saintly or depraved, are worthy of love.
organism, also carry love in their hearts for other people. It is stamped through the DNA. It is the motivation. It is the reason people get out of bed in the morning, or work through their weekends and nights. It is why the wards are clean and the beds are made, why the bloods are taken, the investigations are done, the research is carried out, the people are washed and fed. It is why the hours of study and audit are diligently pursued, it is why the training is so robust, it is why the skills are acquired, it is why the time is given. It is why the NHS was founded in the first place, because all people, no matter how rich or poor, saintly or depraved, are worthy of love.
And yet we find that the human beings who join together to form this body are often struggling with severe stress, anxiety, depression and low morale. How can this be so? Is it possible that the structures we have put in place to try and support this body have instead become a hindrance? When my wife was born she  had congenital talipes aka clubbed feet, due to a positional issue in her mum’s womb. When she was born, her feet were turned in and she had to wear painful calipers for 2 years until she was operated on by a very skillful orthopaedic surgeon. Now, in her mid thirties, she can run and dance because the calipers were taken off in childhood. As the NHS grew and developed, structures were put in place in its formative years to help the right sort of growth and strength to happen, but many of these are no longer useful and in fact are now a hindrance. We have become slaves to serving structures and ways of doing things that work against us as we try and stay true to our core motivation of love.
had congenital talipes aka clubbed feet, due to a positional issue in her mum’s womb. When she was born, her feet were turned in and she had to wear painful calipers for 2 years until she was operated on by a very skillful orthopaedic surgeon. Now, in her mid thirties, she can run and dance because the calipers were taken off in childhood. As the NHS grew and developed, structures were put in place in its formative years to help the right sort of growth and strength to happen, but many of these are no longer useful and in fact are now a hindrance. We have become slaves to serving structures and ways of doing things that work against us as we try and stay true to our core motivation of love.
Part of what we are exploring through ‘Better Care Together’ here in Morecambe Bay is how to dismantle and reform these structures in order to allow this amazing body to function more naturally and freely. This organism is constrained within bizarre silos that make the what and the how of healthcare provision so complex that the why of what we are doing so easily gets forgotten amidst the complexities of service delivery. So, first and foremost, we must recover/rediscover/reconnect with/strengthen our vision, founded upon love and compassion for other people. Galvanized by this vision to provide continually improving, high quality, compassionate and loving healthcare to all in our community, we must tell the structures again and again, that we do not serve them, but they are only there to help us in our task. Right now, they need remodeling, and this is happening. We need less care in hospitals and more in the community, we need better integrated IT, different payment methods, new ways of working in General Practice (in larger more resilient practices, federations or co-operatives) and across the old boundaries, better pathways for patients and communities to be able to care for themselves and each other more effectively. But unless we have love, all these things are like a great symphony orchestra, playing a great new score but void of any connectivity with the audience. The form, as our chief commissioning officer, Hilary Fordham, rightly tells us, must follow the function, but I believe both the form and the function are motivated and under-girded by love and compassion.
in Morecambe Bay is how to dismantle and reform these structures in order to allow this amazing body to function more naturally and freely. This organism is constrained within bizarre silos that make the what and the how of healthcare provision so complex that the why of what we are doing so easily gets forgotten amidst the complexities of service delivery. So, first and foremost, we must recover/rediscover/reconnect with/strengthen our vision, founded upon love and compassion for other people. Galvanized by this vision to provide continually improving, high quality, compassionate and loving healthcare to all in our community, we must tell the structures again and again, that we do not serve them, but they are only there to help us in our task. Right now, they need remodeling, and this is happening. We need less care in hospitals and more in the community, we need better integrated IT, different payment methods, new ways of working in General Practice (in larger more resilient practices, federations or co-operatives) and across the old boundaries, better pathways for patients and communities to be able to care for themselves and each other more effectively. But unless we have love, all these things are like a great symphony orchestra, playing a great new score but void of any connectivity with the audience. The form, as our chief commissioning officer, Hilary Fordham, rightly tells us, must follow the function, but I believe both the form and the function are motivated and under-girded by love and compassion.
So, why Better Care Together? Because the world has changed and the health needs of the population have changed and we simply can’t afford for things to remain as they are. But the deeper reason is so that we can provide continually improving, high quality, compassionate and loving healthcare to ALL in our community. This involves a mindset change. No more can we think of our own little patch. No more can we think ‘I’m just a GP of 1500 patients’, or ‘I’m just a nurse on the cardiology unit’ or I’m just a physio working in one particular area’ or ‘my practice only looks after 17,500 people’ (though of course this kind of personal care is still absolutely vital), but the paradigm shift in our thinking is towards being a member of a healthcare system that cares for the 350,000 people around the Bay. It’s about allow our hearts and our vision to grow bigger whilst giving brilliant care to individuals where we are located. That means learning to work differently, always motivated by the love and compassion we have for people.
Morecambe Bay
 Known for it’s fast moving tides, mud flats, quicksands, islands, rare birds, natural gas, submarine building and nuclear power; Morecambe Bay is a place whose motto is “where beauty surrounds and health abounds”. The first part is true – it is a place with some of the most spectacular views on offer in the entire UK and hidden treasures of wildlife and wonderful walks. A place where I live with my family and I now call home. But it has some of the worst health outcomes in the country, sitting bang in the middle of the North-West – the worst place for health per head of population for any of the regions in the UK. We are the worst for cancer rates, the worst for heart disease, the worst for respiratory problems and the worst for early deaths. And please avoid the rhetoric that would have you believe that it is because of low aspiration and poor choices made by the people here. The North-West is underfunded in terms of health training, according to Health Education England, to the tune of £19 million every year, when compared head to head for other regions. And given the fact that health outcomes are so poor here, it is fascinating that 94% of all health research monies are spent south of Cambridge.
Known for it’s fast moving tides, mud flats, quicksands, islands, rare birds, natural gas, submarine building and nuclear power; Morecambe Bay is a place whose motto is “where beauty surrounds and health abounds”. The first part is true – it is a place with some of the most spectacular views on offer in the entire UK and hidden treasures of wildlife and wonderful walks. A place where I live with my family and I now call home. But it has some of the worst health outcomes in the country, sitting bang in the middle of the North-West – the worst place for health per head of population for any of the regions in the UK. We are the worst for cancer rates, the worst for heart disease, the worst for respiratory problems and the worst for early deaths. And please avoid the rhetoric that would have you believe that it is because of low aspiration and poor choices made by the people here. The North-West is underfunded in terms of health training, according to Health Education England, to the tune of £19 million every year, when compared head to head for other regions. And given the fact that health outcomes are so poor here, it is fascinating that 94% of all health research monies are spent south of Cambridge.
Looking at the health system here, it would be easy to be disheartened. The recent Kirkup enquiry into drastic failures at the University Hospitals of Morecambe Bay Foundation Trust, to which the trust has responded with humility and learning, highlighted just how much change is needed here. We also face the vast complexities associated with local tariff modification. And as if the local challenges are not enough, we have the added recruitment crisis that is affecting the entire country (worse in rural areas), the undermining of our junior doctors and their pay, the berating of nursing colleagues from overseas who don’t get paid enough to remain here, severely low morale in the system as a whole, and a maltreatment of General Practice in the National Press at a time when the profession is on the ropes; then there is the huge debt of the hospital trusts – compounded by the PFI fiasco and the creeping privatisation of our services, which has led to the shambles that is out of hours care and staffing issues due to agency working. And 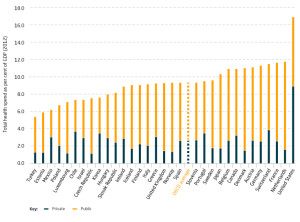 all that is on the background of a hugely underfunded healthservice, with only 8.5% of GDP spent on health compared to the 11% most other OECD countries spend. The truth is, we simply do not spend enough of our GDP on health care for it to be sustainable in its current form, and the government knows this.
all that is on the background of a hugely underfunded healthservice, with only 8.5% of GDP spent on health compared to the 11% most other OECD countries spend. The truth is, we simply do not spend enough of our GDP on health care for it to be sustainable in its current form, and the government knows this.
For the last three and a half years, I have been working here as a GP, having previously spent 14 years in Manchester. Three days a week, I work clinically in my practice, and the rest of my work time is given over to being part of the executive team for the Lancashire North CCG – I am the lead for Health and Wellbeing. Although the odds are stacked against us, something really wonderful is stirring here. I would go as far to say that believe it or not, Morecambe Bay is one of the most exciting places to be involved in health and social care anywhere in the UK. Let me tell you why I feel so hopeful (and why you should consider working here)!
Understanding the Purpose of Healthcare
 A chap called, Phil Cass, who is an (unmet) hero of mine in the medical field, lives in the state of Ohio. He has been been doing some work with local communities to try and make healthcare affordable for everybody – a truly noble quest in a country where 50 million people cannot afford any. He took the conversation out to the community and they tried various questions, but found they weren’t really getting anywhere. He and team of people then realised that they needed to ask a better question. The question they needed to get to was “What is the PURPOSE of our healthcare system?” – Once the communities began engaging with this question, something remarkable happened – time and again, the same answer came through – the answer was this:- “to provide OPTIMAL healthcare to everybody.” The word optimal recognised that every person would achieve different “levels” of health depending on age, underlying health problems, genetics etc, but the vision of the community became that they wanted every individual and the community as a whole to live as well as they could. The community then realised that in order for this to be achievable, they had to fundamentally change their relationship with the healthcare system and this then made care much more affordable. Here in Morecambe Bay, we are taking a similar conversation to the 320000 citizens who live here.
A chap called, Phil Cass, who is an (unmet) hero of mine in the medical field, lives in the state of Ohio. He has been been doing some work with local communities to try and make healthcare affordable for everybody – a truly noble quest in a country where 50 million people cannot afford any. He took the conversation out to the community and they tried various questions, but found they weren’t really getting anywhere. He and team of people then realised that they needed to ask a better question. The question they needed to get to was “What is the PURPOSE of our healthcare system?” – Once the communities began engaging with this question, something remarkable happened – time and again, the same answer came through – the answer was this:- “to provide OPTIMAL healthcare to everybody.” The word optimal recognised that every person would achieve different “levels” of health depending on age, underlying health problems, genetics etc, but the vision of the community became that they wanted every individual and the community as a whole to live as well as they could. The community then realised that in order for this to be achievable, they had to fundamentally change their relationship with the healthcare system and this then made care much more affordable. Here in Morecambe Bay, we are taking a similar conversation to the 320000 citizens who live here.
Starting and Finishing with People
The NHS has become a horribly target driven culture and amidst the stress and strain, in which staff themselves often feel dehumanised, it is easy to forget what we are here for – human beings. Putting people (rather than patients) at the heart of how we think about health is a vital starting point.
 So, we are learning to truly engage with and listen to the people here. With the help of an amazng team, I have been hosting conversations here in Carnforth, in the form of ‘World Cafe’ discussions (a fantastic way to ensure every voice is heard). Our hope is that from Millom to Morecambe, we will see conversations springing up as we talk about how Morecambe Bay can become the healthiest place in the UK. And by being healthy, we do not mean just physical health. We are talking about mental health, social health (there really is such a thing as society!) and systemic health (including issues like road safety – still the biggest cause of death for our children, the environment and pollution, the real effects of austerity on our communities, the power of advertising and the high cost of healthy food). And as we talk with our citizens, we are not coming in with ideas of how to fix things, as though we are some kind of experts. People are the experts in themselves the their communities, and we have some expertise in a variety of fields. So, we have a meeting of equals. We are waiting to see what rises within the communities themselves and looking to support initiatives where that is wanted. Communities are having some really exciting conversations and some people are standing up to become ‘health and well-being champions’ (the photo is taken from a recent event, supported by our Mayor in Carnforth, looking to do exactly that), who want to help steward the well-being of the community and the environment. It is incredible to see how many people want to get more involved with making this area more “healthy”. Volunteers are springing up with ideas like gorilla gardening, shopping for elderly neighbours, cooking meals for those coming out of hospital, setting up choirs, starting youth clubs, community transport services to help housebound people get to appointments, cleaning up our streets, creating safe parks and being hands on with support for those receiving palliative care. People are learning to ‘self-care’ and care for each other more effectively.
So, we are learning to truly engage with and listen to the people here. With the help of an amazng team, I have been hosting conversations here in Carnforth, in the form of ‘World Cafe’ discussions (a fantastic way to ensure every voice is heard). Our hope is that from Millom to Morecambe, we will see conversations springing up as we talk about how Morecambe Bay can become the healthiest place in the UK. And by being healthy, we do not mean just physical health. We are talking about mental health, social health (there really is such a thing as society!) and systemic health (including issues like road safety – still the biggest cause of death for our children, the environment and pollution, the real effects of austerity on our communities, the power of advertising and the high cost of healthy food). And as we talk with our citizens, we are not coming in with ideas of how to fix things, as though we are some kind of experts. People are the experts in themselves the their communities, and we have some expertise in a variety of fields. So, we have a meeting of equals. We are waiting to see what rises within the communities themselves and looking to support initiatives where that is wanted. Communities are having some really exciting conversations and some people are standing up to become ‘health and well-being champions’ (the photo is taken from a recent event, supported by our Mayor in Carnforth, looking to do exactly that), who want to help steward the well-being of the community and the environment. It is incredible to see how many people want to get more involved with making this area more “healthy”. Volunteers are springing up with ideas like gorilla gardening, shopping for elderly neighbours, cooking meals for those coming out of hospital, setting up choirs, starting youth clubs, community transport services to help housebound people get to appointments, cleaning up our streets, creating safe parks and being hands on with support for those receiving palliative care. People are learning to ‘self-care’ and care for each other more effectively.
 Atul Gawande, another hero, has written powerfully in his book ‘Being Mortal’ (a manifesto for change in how the medical profession deals with the whole topic of death). It challenges the ways in which we don’t face up to our mortality very well. We end up spending an inordinate amount of money in the last year of someone’s life on drugs which have a lottery-ticket chance of working, when all the time, we could help people live longer and more comfortably if we introduced
Atul Gawande, another hero, has written powerfully in his book ‘Being Mortal’ (a manifesto for change in how the medical profession deals with the whole topic of death). It challenges the ways in which we don’t face up to our mortality very well. We end up spending an inordinate amount of money in the last year of someone’s life on drugs which have a lottery-ticket chance of working, when all the time, we could help people live longer and more comfortably if we introduced hospice care earlier and treated people with compassion. We are looking to launch compassionate communities here, where we are not afraid to talk about the difficult issues of life. We want people to have the kind of care that allows them to make supported choices to live well, right to the end. Our BCT Matron, Alison Scott, is a true champion of this cause, along with Dr Pete Nightingale, the recent RCGP national lead of palliative care, Dr Nick Sayer, Palliative Care Consultant and Sue McGraw, CEO of St John’s Hospice.
hospice care earlier and treated people with compassion. We are looking to launch compassionate communities here, where we are not afraid to talk about the difficult issues of life. We want people to have the kind of care that allows them to make supported choices to live well, right to the end. Our BCT Matron, Alison Scott, is a true champion of this cause, along with Dr Pete Nightingale, the recent RCGP national lead of palliative care, Dr Nick Sayer, Palliative Care Consultant and Sue McGraw, CEO of St John’s Hospice.
From the moment of conception to the moment of death, we want people to have optimal health in Morecambe Bay. We want people to be able to live well in the context of sometimes very disabling and difficult circumstances and illness. We want to see care wrapped around a person, recognising that this cannot always be provided for by the current ‘system’.
Better Care Together
 Before the government launched its five year forward view for the NHS, we were already in the process of learning to work very differently here, around the Bay. We have been blurring the boundaries between various care organisations (including the acute trust, the mental health trust, the GP practices – now forming into a more cohesive federation, community nursing in its various forms, the police, the fire-service, local schools, the voluntary sector, the county council and social services), building relationships between clinical leaders, sharing the burdens of financial choices and care conundrums, strengthening the pillars of the various players, redesigning care pathways across the clinical spectrum to ensure better care for patients and infusing everything we do with integrated IT.
Before the government launched its five year forward view for the NHS, we were already in the process of learning to work very differently here, around the Bay. We have been blurring the boundaries between various care organisations (including the acute trust, the mental health trust, the GP practices – now forming into a more cohesive federation, community nursing in its various forms, the police, the fire-service, local schools, the voluntary sector, the county council and social services), building relationships between clinical leaders, sharing the burdens of financial choices and care conundrums, strengthening the pillars of the various players, redesigning care pathways across the clinical spectrum to ensure better care for patients and infusing everything we do with integrated IT.
The creation of integrated care communities (ICC) is at the heart of the vision to transfer more care out of the hospital setting and back into the community, whilst ensuring that the funding follows the patient. Our care co-ordinators become the new first port of call for our most vulnerable or ‘at-risk-of-admisison’ citizens. The idea is to wrap care around a person in the community, with the appropriate services being called in. Many times a care coordinator can bring in help from allied professions/volunteers and avoid unnecessary admissions or overlap of services. This means less pressure on the Emergency department and less pressure on General practice. We are also working to ensure our Urgent Care provision is fit for purpose with GPs, NWAS (our ambulance/paramedic service) and Out of Hours care offering much more of a buffer for our Emergency Departments.
Radical Leadership and the Challenges Ahead
There are many challenges ahead and both local and national threats remain. We are steering a huge ship through an iceberg field, and the so the waters are dangerous. We risk a lack of transfer of funding towards General Practice making it difficult for appropriate ‘buy-in’ for the changes we need to see. GPs ourselves have some brave leaps of faith to make. We will not be able to guarantee more money in our own pockets, but we must decide between protecting what we know or federating more fully for a more sustainable and excellent provision of care in the future (providing better education and career development in the process). We risk disengagement from senior clinicians in our hospital trust if the vision is not fully owned and shared by all. We have huge risks associated with the truly shocking cuts being forced upon our county council and a destabilisation of social care. We risk our nursing care home provision causing a halt to the entire program due to the vast complexities involved. Political whims, rules and pressures often seems to knock the wind out of our sails and could still utterly destabilise and destroy what is tenderly being built here.
 However, one of the things which I have found most encouraging here is the quality and attitude of the leadership. Andrew Bennett as the SRO for BCT and
However, one of the things which I have found most encouraging here is the quality and attitude of the leadership. Andrew Bennett as the SRO for BCT and  Jackie Daniels, the CEO of UHMBT (the acute trust), have built stunning teams of people! I have the privilege of sitting on the executive board for the CCG and we have exec to exec meetings with the acute trust, in particular. The truth about Better Care Together is that for some it may mean doing themselves out of a job, letting go of power, and choosing facilitation and servanthood over domination and self-preservation. Leadership that is determined by the future and is able to lay itself down for the sake of what is really needed in our communities is exactly the kind of leadership we need. The leadership here across the spectrum is brave, it is altruistic, it is kenarchic, it is relational and it is rooted in the community.
Jackie Daniels, the CEO of UHMBT (the acute trust), have built stunning teams of people! I have the privilege of sitting on the executive board for the CCG and we have exec to exec meetings with the acute trust, in particular. The truth about Better Care Together is that for some it may mean doing themselves out of a job, letting go of power, and choosing facilitation and servanthood over domination and self-preservation. Leadership that is determined by the future and is able to lay itself down for the sake of what is really needed in our communities is exactly the kind of leadership we need. The leadership here across the spectrum is brave, it is altruistic, it is kenarchic, it is relational and it is rooted in the community.
And so we press on, knowing that we cannot remain as we are, knowing that in building together with our communities, we are finding that the future is not as bleak as it might otherwise be. Together we are wiser, braver and kinder. Morecambe Bay is no longer the butt of the jokes. It is becoming a place of hope, a place of potential, a light that is beginning to burn, dare I say it – a place shaped by love. It will be a place where health abounds in the beauty that surrounds.