A few months ago I wrote a blog suggesting the right approach for the junior doctors was one of subversion and submission. But I think I was wrong. It’s not that I’ve changed my mind on the power of subversion and submission, it’s just that this entire spectacle surrounding the junior doctors, the ‘7 day NHS’, the strikes and the media reporting there of actually affects us all at a profound level.
 This situation exposes something far deeper than just an argument between Jeremy Hunt and the BMA and is far more important than discovering who has the strongest will power. Infact, the BMA have made a major error in targeting Jeremy Hunt so vindictively, because in the final analysis, this isn’t about Hunt at all. Jeremy Hunt can be replaced in a moment, and is likely to be succeeded by a far more robust
This situation exposes something far deeper than just an argument between Jeremy Hunt and the BMA and is far more important than discovering who has the strongest will power. Infact, the BMA have made a major error in targeting Jeremy Hunt so vindictively, because in the final analysis, this isn’t about Hunt at all. Jeremy Hunt can be replaced in a moment, and is likely to be succeeded by a far more robust  Boris Johnson, who will simply pound his fist more visciously. To make Hunt the scape goat narrows this debate to something far too insignificant and actually strengthens the government’s ability to do exactly as they please.
Boris Johnson, who will simply pound his fist more visciously. To make Hunt the scape goat narrows this debate to something far too insignificant and actually strengthens the government’s ability to do exactly as they please.
Sadly, however, all this proves is how defunct our current system of government has always been. What the government really want is a discussion about how we can improve patient access across the weekend timeframe. However, what they did was to decide this is necessary and went ahead to try to fix what is incredibly complex. There was no discssion, no real engagement, no conversation, no asking of the deep questions. Just because we want something, doesn’t mean we can have it! Just because we think something is a good idea, doesn’t mean everyone else will agree! The entire process of enagement and change management is not understood at all. In the first place, the goverment could instead have said to all the hospital trusts across the country what their hopes and intentions were and then waited to see if this was workable, in what way and how much it would cost. But you cannot simply act like Pharoah and expect the brick makers to make ever more bricks with less and less resource available – otherwise, you face an exodus!
place, the goverment could instead have said to all the hospital trusts across the country what their hopes and intentions were and then waited to see if this was workable, in what way and how much it would cost. But you cannot simply act like Pharoah and expect the brick makers to make ever more bricks with less and less resource available – otherwise, you face an exodus!
What this entire debacle demonstrates is just how far free market capitalism has gone in its use of people as biopower to drive the system. The junior doctors of the NHS are nothing more than fodder to make the machine run. It doesn’t matter at all to the government that their lovely idea of a ‘7 day NHS’ is both unaffordable (due to chronic underinvestment in the health service) and unstaffable (due to a combination of under-training of staff across the board, and free market forces which work against people remaining in the UK). What this exposes in its most blatant form, is the chronic and shocking abuse of power, because of the very structures we have in place and the foundations upon which our society is built – namely violence, debt and control. And so, we see the human being reduced to what Hardt and Negri call ‘naked life’.
 The system, to which we must all bow doesn’t care for the needs of the people who work within it. It will force them to submit. Why should doctors (many of whom work for less than the minimum wage, when on call) be allowed time to rest at weekends? Why can’t everybody have routine care through the weekend, just as from monday to friday (even though most of our top clinicians think we need better emergency care and not routine access)? Surely our economy needs this kind of health service? And actually, whilst we’re on it, isn’t it a waste of time, allowing teachers to have weekends off as well? Don’t we need our children to work harder, or at least be given some sort of babysitting service, so we can get more for our pound of flesh from their parents? If we are to have a 24/7 health service, why not a 24/7 education service? Our shops are already open practically 24/7. In this commercial world – shouldn’t everything else follow suit? No, no and NO!!
The system, to which we must all bow doesn’t care for the needs of the people who work within it. It will force them to submit. Why should doctors (many of whom work for less than the minimum wage, when on call) be allowed time to rest at weekends? Why can’t everybody have routine care through the weekend, just as from monday to friday (even though most of our top clinicians think we need better emergency care and not routine access)? Surely our economy needs this kind of health service? And actually, whilst we’re on it, isn’t it a waste of time, allowing teachers to have weekends off as well? Don’t we need our children to work harder, or at least be given some sort of babysitting service, so we can get more for our pound of flesh from their parents? If we are to have a 24/7 health service, why not a 24/7 education service? Our shops are already open practically 24/7. In this commercial world – shouldn’t everything else follow suit? No, no and NO!!
 This is why we need a revolution of solidarity and resistance. We need a people movement who will stand together and be brave enough to say that there is a different way to see the world and a new way to live within it. Our naked life itself, although currently abused, can become for us our greatest power. Our naked life can expose the truth of just how abusive our systems have become. Our naked life, when combined with the indestructable force of kenotic love, becomes the very agent of change that we need.
This is why we need a revolution of solidarity and resistance. We need a people movement who will stand together and be brave enough to say that there is a different way to see the world and a new way to live within it. Our naked life itself, although currently abused, can become for us our greatest power. Our naked life can expose the truth of just how abusive our systems have become. Our naked life, when combined with the indestructable force of kenotic love, becomes the very agent of change that we need.
So, what next for the junior doctors? Should they strike next week, including for emergency care? Are they ready for the media (who have lost the art of journalism) to turn against them? Are they ready for the storm that will ensue? Well, lives have already very sadly been lost. How many more can stand under the strain? What if the public turn against their heros?
It is time for something deeper to take place. It is time for solidarity. It is time for those of us in senior positions to cover shifts and show our unreserved support. It is time for the public, not just teachers, but across the board, to stand with the juniors. As my friend, Julie Tomlin showed me, we have to learn from the arab spring that one march alone will not do it. March after march after march may be needed. And singing too!! Let songs be heard on the streets! And to  really demonstrate the power of naked life……how about naked marches?!! (I grew up in Coventry, and so the story of Lady Godiva is in my blood – nakedness overcame oppression once before!). Or maybe the staff of the NHS should all turn up to work with no clothes on?!! How about people stripping off at least to their underwear to expose both the fragility and the power of naked life?!
really demonstrate the power of naked life……how about naked marches?!! (I grew up in Coventry, and so the story of Lady Godiva is in my blood – nakedness overcame oppression once before!). Or maybe the staff of the NHS should all turn up to work with no clothes on?!! How about people stripping off at least to their underwear to expose both the fragility and the power of naked life?!
There is a different way for humanity. We can free ourselves from the oppressive yolk that seeks to divide and rule us. Perhaps, the Junior Doctors could be more creative and expose the deep structures of oppression that lie beneath the calls for this ‘7 day NHS’? Now is the time for subversion, for exposing just how unjust our systems are. But subversion alone will not suffice. We need solidarity and resistance. So, who will stand and march with the Junior Doctors (naked if need be?!) for an altogether different future?
 This situation exposes something far deeper than just an argument between Jeremy Hunt and the BMA and is far more important than discovering who has the strongest will power. Infact, the BMA have made a major error in targeting Jeremy Hunt so vindictively, because in the final analysis, this isn’t about Hunt at all. Jeremy Hunt can be replaced in a moment, and is likely to be succeeded by a far more robust
This situation exposes something far deeper than just an argument between Jeremy Hunt and the BMA and is far more important than discovering who has the strongest will power. Infact, the BMA have made a major error in targeting Jeremy Hunt so vindictively, because in the final analysis, this isn’t about Hunt at all. Jeremy Hunt can be replaced in a moment, and is likely to be succeeded by a far more robust  Boris Johnson, who will simply pound his fist more visciously. To make Hunt the scape goat narrows this debate to something far too insignificant and actually strengthens the government’s ability to do exactly as they please.
Boris Johnson, who will simply pound his fist more visciously. To make Hunt the scape goat narrows this debate to something far too insignificant and actually strengthens the government’s ability to do exactly as they please. place, the goverment could instead have said to all the hospital trusts across the country what their hopes and intentions were and then waited to see if this was workable, in what way and how much it would cost. But you cannot simply act like Pharoah and expect the brick makers to make ever more bricks with less and less resource available – otherwise, you face an exodus!
place, the goverment could instead have said to all the hospital trusts across the country what their hopes and intentions were and then waited to see if this was workable, in what way and how much it would cost. But you cannot simply act like Pharoah and expect the brick makers to make ever more bricks with less and less resource available – otherwise, you face an exodus! The system, to which we must all bow doesn’t care for the needs of the people who work within it. It will force them to submit. Why should doctors (many of whom work for less than the minimum wage, when on call) be allowed time to rest at weekends? Why can’t everybody have routine care through the weekend, just as from monday to friday (even though most of our top clinicians think we need better emergency care and not routine access)? Surely our economy needs this kind of health service? And actually, whilst we’re on it, isn’t it a waste of time, allowing teachers to have weekends off as well? Don’t we need our children to work harder, or at least be given some sort of babysitting service, so we can get more for our pound of flesh from their parents? If we are to have a 24/7 health service, why not a 24/7 education service? Our shops are already open practically 24/7. In this commercial world – shouldn’t everything else follow suit? No, no and NO!!
The system, to which we must all bow doesn’t care for the needs of the people who work within it. It will force them to submit. Why should doctors (many of whom work for less than the minimum wage, when on call) be allowed time to rest at weekends? Why can’t everybody have routine care through the weekend, just as from monday to friday (even though most of our top clinicians think we need better emergency care and not routine access)? Surely our economy needs this kind of health service? And actually, whilst we’re on it, isn’t it a waste of time, allowing teachers to have weekends off as well? Don’t we need our children to work harder, or at least be given some sort of babysitting service, so we can get more for our pound of flesh from their parents? If we are to have a 24/7 health service, why not a 24/7 education service? Our shops are already open practically 24/7. In this commercial world – shouldn’t everything else follow suit? No, no and NO!! This is why we need a revolution of solidarity and resistance. We need a people movement who will stand together and be brave enough to say that there is a different way to see the world and a new way to live within it. Our naked life itself, although currently abused, can become for us our greatest power. Our naked life can expose the truth of just how abusive our systems have become. Our naked life, when combined with the indestructable force of kenotic love, becomes the very agent of change that we need.
This is why we need a revolution of solidarity and resistance. We need a people movement who will stand together and be brave enough to say that there is a different way to see the world and a new way to live within it. Our naked life itself, although currently abused, can become for us our greatest power. Our naked life can expose the truth of just how abusive our systems have become. Our naked life, when combined with the indestructable force of kenotic love, becomes the very agent of change that we need. really demonstrate the power of naked life……how about naked marches?!! (I grew up in Coventry, and so the story of Lady Godiva is in my blood – nakedness overcame oppression once before!). Or maybe the staff of the NHS should all turn up to work with no clothes on?!! How about people stripping off at least to their underwear to expose both the fragility and the power of naked life?!
really demonstrate the power of naked life……how about naked marches?!! (I grew up in Coventry, and so the story of Lady Godiva is in my blood – nakedness overcame oppression once before!). Or maybe the staff of the NHS should all turn up to work with no clothes on?!! How about people stripping off at least to their underwear to expose both the fragility and the power of naked life?! If I were to design a health centre, it would not look like any of the places I work in. They are all far too clinical and are probably not very conducive to healing. For starters, there would be a whole lot more natural light, with beautiful artwork (I have some amazing pieces in my room now, by a brilliant local artist, Emma Hamilton) and sense of a continuum with the landscape. There would be places for people to talk with each other around tables where food and drink could be served, isolation broken and community restored. There would be places to encourage exercise or mindfulness through colouring. My room would have a piano in the corner and it would be filled with art, poems, quotes and there would be huge windows with magnificent views of the sea.
If I were to design a health centre, it would not look like any of the places I work in. They are all far too clinical and are probably not very conducive to healing. For starters, there would be a whole lot more natural light, with beautiful artwork (I have some amazing pieces in my room now, by a brilliant local artist, Emma Hamilton) and sense of a continuum with the landscape. There would be places for people to talk with each other around tables where food and drink could be served, isolation broken and community restored. There would be places to encourage exercise or mindfulness through colouring. My room would have a piano in the corner and it would be filled with art, poems, quotes and there would be huge windows with magnificent views of the sea. who I am. Even now, I spend a lot of time laughing with my patients. Laughter is so good! It is healing in and of itself. There would be time for music. I would sing to my patients (they might well leave faster!)……Every doctor I know has talents, gifts, hobbies, and hidden depths that are rarely used when they encounter their patients. I wonder how much more effective we might be as healers, if we reconnected with the God-given sense of who we are and what makes our own hearts sing.
who I am. Even now, I spend a lot of time laughing with my patients. Laughter is so good! It is healing in and of itself. There would be time for music. I would sing to my patients (they might well leave faster!)……Every doctor I know has talents, gifts, hobbies, and hidden depths that are rarely used when they encounter their patients. I wonder how much more effective we might be as healers, if we reconnected with the God-given sense of who we are and what makes our own hearts sing. I’m not a great meetings person. I just generally find them tedious. I lose concentration easily, I get distracted, I end up thinking about a whole lot of things that maybe I shouldn’t be thinking about or eat far too many biscuits and then feel bloated and guilty at the same time! Meetings and me don’t really mix….but I have to go to a lot of them, in fact, I now have to chair many of them and so I’ve been on a bit of a journey about how meetings can be made better.
I’m not a great meetings person. I just generally find them tedious. I lose concentration easily, I get distracted, I end up thinking about a whole lot of things that maybe I shouldn’t be thinking about or eat far too many biscuits and then feel bloated and guilty at the same time! Meetings and me don’t really mix….but I have to go to a lot of them, in fact, I now have to chair many of them and so I’ve been on a bit of a journey about how meetings can be made better. is not that they don’t achieve anything. Nor is it that I’m involved in conversations I don’t care about – actually I don’t go to any meetings in which I don’t deeply care about the things being discussed. So what is my problem? My problem is that meetings, and I don’t think this is unique to the NHS (but this is where most of my meetings take place), are so often devoid of any real human connection. They lack care for those attending the meetings. It’s so easy to get so focussed on the stuff, the business, the discussions, the problems, that we forget that there are other human beings in the room, each of whom arrive in the room (or virtual space) with many different emotions, stories, dreams and realities that may be really important, but we don’t know because we don’t give space to those things.
is not that they don’t achieve anything. Nor is it that I’m involved in conversations I don’t care about – actually I don’t go to any meetings in which I don’t deeply care about the things being discussed. So what is my problem? My problem is that meetings, and I don’t think this is unique to the NHS (but this is where most of my meetings take place), are so often devoid of any real human connection. They lack care for those attending the meetings. It’s so easy to get so focussed on the stuff, the business, the discussions, the problems, that we forget that there are other human beings in the room, each of whom arrive in the room (or virtual space) with many different emotions, stories, dreams and realities that may be really important, but we don’t know because we don’t give space to those things. a simple technique from the ‘art of hosting’ I give space for a ‘check-in’. A check in is really simple, it’s just what it says on the tin. There are usually 2 questions and they can vary from meeting to meeting. Often, I just ask: How are you? And what do you love about your job? It is so important to know how each other is doing, so we can create teams that care for each other. People don’t have to be honest, but when they choose to be vulnerable, it opens up a space that is incredible and invites the entire team to go a bit deeper. And giving space for people to focus on the positive aspects of their work automatically changes the dynamic of any meeting from the start. Another of my favourite questions is: What do you love about working with the person on your left? (And if there’s time another round of ‘And what else do you love about working with the person on your left?). It is so healthy for a team to learn to appreciate one another but more than that, to actually tell each other that they are valued. You can get to know one another over a period of just a few weeks so much more and you end up actually caring about one another’s lives and wellbeing.
a simple technique from the ‘art of hosting’ I give space for a ‘check-in’. A check in is really simple, it’s just what it says on the tin. There are usually 2 questions and they can vary from meeting to meeting. Often, I just ask: How are you? And what do you love about your job? It is so important to know how each other is doing, so we can create teams that care for each other. People don’t have to be honest, but when they choose to be vulnerable, it opens up a space that is incredible and invites the entire team to go a bit deeper. And giving space for people to focus on the positive aspects of their work automatically changes the dynamic of any meeting from the start. Another of my favourite questions is: What do you love about working with the person on your left? (And if there’s time another round of ‘And what else do you love about working with the person on your left?). It is so healthy for a team to learn to appreciate one another but more than that, to actually tell each other that they are valued. You can get to know one another over a period of just a few weeks so much more and you end up actually caring about one another’s lives and wellbeing.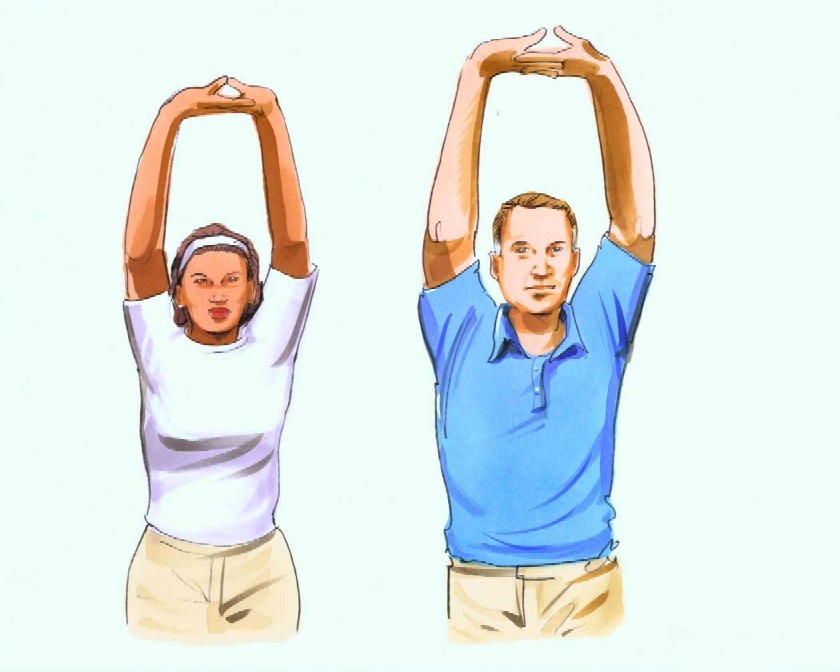 University of East London. In the department of positive psychology there, a bell goes every 25 minutes of a lecture and everybody stands up and has a stretch. Research clearly shows, we don’t concentrate for any more than 25 minutes. And so now, in my meetings, every 25 minutes, my alarm goes off and we all stand up and stretch and get the blood flowing round our bodies. We’ve become so conditioned, like Pavlov’s dogs, that if anyone’s phone goes we all start to stand and stretch! Plus, it is great for low back pain!
University of East London. In the department of positive psychology there, a bell goes every 25 minutes of a lecture and everybody stands up and has a stretch. Research clearly shows, we don’t concentrate for any more than 25 minutes. And so now, in my meetings, every 25 minutes, my alarm goes off and we all stand up and stretch and get the blood flowing round our bodies. We’ve become so conditioned, like Pavlov’s dogs, that if anyone’s phone goes we all start to stand and stretch! Plus, it is great for low back pain! in the middle of a meeting. Using a very simple technique, I encourage everyone to find a comfortable sitting position. We then breathe in through our noses for the count of 4, deliberately breathing a sense of hope, peace, love and gratitude. We then hold this and hold our breath for the count of 8 (people count at their own pace) and then breathe out to through our mouths for the count of 8. When we breathe out, we deliberately breathe out stress, bitterness, anger, distraction, or anything that stops us being able to connect. And then we continue. The first few times I tried this, we had some giggling (mainly from me), photos being posted on twitter (!) and general weird feelings…..but we have pushed through and it’s amazing how good it feels to just stop and be and let the busyness just wash over us for a couple of minutes.
in the middle of a meeting. Using a very simple technique, I encourage everyone to find a comfortable sitting position. We then breathe in through our noses for the count of 4, deliberately breathing a sense of hope, peace, love and gratitude. We then hold this and hold our breath for the count of 8 (people count at their own pace) and then breathe out to through our mouths for the count of 8. When we breathe out, we deliberately breathe out stress, bitterness, anger, distraction, or anything that stops us being able to connect. And then we continue. The first few times I tried this, we had some giggling (mainly from me), photos being posted on twitter (!) and general weird feelings…..but we have pushed through and it’s amazing how good it feels to just stop and be and let the busyness just wash over us for a couple of minutes.

 een willing to be humble and be impacted by these stories. I am grateful for relationships and partnerships that are being established between those of us who provide services and those who use them. I am grateful for the tenacity of people who want to see our cultures change. I am grateful for ‘The Leeds Poverty Truth Challenge’ and its far reaching consequences. I am grateful for the opportunity to break down barriers and find positive ways forward. I am grateful for the transformative power of listening and the change that can happen when we really encounter another human being. Better Care Together is so much better when we work together with those we are trying to serve.
een willing to be humble and be impacted by these stories. I am grateful for relationships and partnerships that are being established between those of us who provide services and those who use them. I am grateful for the tenacity of people who want to see our cultures change. I am grateful for ‘The Leeds Poverty Truth Challenge’ and its far reaching consequences. I am grateful for the opportunity to break down barriers and find positive ways forward. I am grateful for the transformative power of listening and the change that can happen when we really encounter another human being. Better Care Together is so much better when we work together with those we are trying to serve. Amidst the current ‘efficiency savings’, or cuts by any other name, in the NHS, the voluntary or 3rd sector, including the faith communities are an absolutely vital partner in health and social care. Here in Morecambe Bay, we are seeing incredible work done by this sector. Genuinely, the safety net created across this Bay for people with significant mental health issues, chronic physical health complaints, those at the end of life, the isolated and lonely etc is amazing. However, as the financial squeeze increases on the NHS, the 3rd sector, although phenomenally resilient and full of social entrepreneurs with good heart, is really beginning to struggle to secure funding. If the 3rd sector, (which gives far more for far less) begins to crumble, then we will see health and social care completely collapse.
Amidst the current ‘efficiency savings’, or cuts by any other name, in the NHS, the voluntary or 3rd sector, including the faith communities are an absolutely vital partner in health and social care. Here in Morecambe Bay, we are seeing incredible work done by this sector. Genuinely, the safety net created across this Bay for people with significant mental health issues, chronic physical health complaints, those at the end of life, the isolated and lonely etc is amazing. However, as the financial squeeze increases on the NHS, the 3rd sector, although phenomenally resilient and full of social entrepreneurs with good heart, is really beginning to struggle to secure funding. If the 3rd sector, (which gives far more for far less) begins to crumble, then we will see health and social care completely collapse. A second solution could be for the 3rd Sector to form one or several larger co-operatives. The huge advantage here is that it would then allow a more straight forward commissioning relationship and would allow the many to be become stronger and more resilient together. In a co-operative model, it would be easier to build research partnerships and accountability between members. It would also give the sector more clout as a partner round the table with the various public sector organisations.
A second solution could be for the 3rd Sector to form one or several larger co-operatives. The huge advantage here is that it would then allow a more straight forward commissioning relationship and would allow the many to be become stronger and more resilient together. In a co-operative model, it would be easier to build research partnerships and accountability between members. It would also give the sector more clout as a partner round the table with the various public sector organisations. If you take the work of Steve Peters (of “The Chimp Paradox” fame) seriously, which I do, then you can see Chimps at work everywhere in the NHS right now (and I’m not taking a cheap shot at Jeremy Hunt). For those of you, who have no idea what I’m talking about, then do read the book….but a brief precis is this: each of us are two people – we are both simultaneously an emotionally driven, primal chimp and a more rational human being. When faced with difficult circumstances, our chimps all too easily take over and our behaviour is driven by our emotions, because our human also feels insecure and we lose hold of our values (the computer part of our brains) which is able to alter our chimp behaviour.
If you take the work of Steve Peters (of “The Chimp Paradox” fame) seriously, which I do, then you can see Chimps at work everywhere in the NHS right now (and I’m not taking a cheap shot at Jeremy Hunt). For those of you, who have no idea what I’m talking about, then do read the book….but a brief precis is this: each of us are two people – we are both simultaneously an emotionally driven, primal chimp and a more rational human being. When faced with difficult circumstances, our chimps all too easily take over and our behaviour is driven by our emotions, because our human also feels insecure and we lose hold of our values (the computer part of our brains) which is able to alter our chimp behaviour. feel about what is happening in General Practice, Community Nursing/Therapy and indeed the NHS at large and it becomes easy to function out of raw emotion, heading into ‘rant mode’ or a strong defensive posture with the rest of my pride. But I have found it brings division. It pits my practice against another or General Practice at scale against the Hospital Trust or the government or whoever. But it doesn’t actually solve anything. It stares the problem in the face and hollers at it or throws faeces at it, and other than being cathartic (which has it’s place for a while), it doesn’t engage with a creative or collaborative process about how we face the future. The facts are right in front of us, and there is some thought about how to make General Practice strong enough to survive, be that through giant mergers or the formation of federations. Here in Morecambe Bay, we are experimenting with both those options and also trying to work in Integrated Care Communities (incorporating all our community partners) according to geographical locations.
feel about what is happening in General Practice, Community Nursing/Therapy and indeed the NHS at large and it becomes easy to function out of raw emotion, heading into ‘rant mode’ or a strong defensive posture with the rest of my pride. But I have found it brings division. It pits my practice against another or General Practice at scale against the Hospital Trust or the government or whoever. But it doesn’t actually solve anything. It stares the problem in the face and hollers at it or throws faeces at it, and other than being cathartic (which has it’s place for a while), it doesn’t engage with a creative or collaborative process about how we face the future. The facts are right in front of us, and there is some thought about how to make General Practice strong enough to survive, be that through giant mergers or the formation of federations. Here in Morecambe Bay, we are experimenting with both those options and also trying to work in Integrated Care Communities (incorporating all our community partners) according to geographical locations. If we are going to find solutions to the needs of the people we serve and develop together (no matter what is being shaped from the centre) a future healthcare model that works, GPs may need to let go of our power, as we have known it and embrace a different way of being. I think a possible solution lies with the co-operative movement as this would allow a truly integrative model to develop that benefits all our workers, no matter what their role, giving us the cultural environment in which innovation, excellence, learning, creativity and compassion could really flourish. Due to the nature of co-operatives and the principles at their core, a powerful force could be released which provides alternative solutions for a more equitable society.
If we are going to find solutions to the needs of the people we serve and develop together (no matter what is being shaped from the centre) a future healthcare model that works, GPs may need to let go of our power, as we have known it and embrace a different way of being. I think a possible solution lies with the co-operative movement as this would allow a truly integrative model to develop that benefits all our workers, no matter what their role, giving us the cultural environment in which innovation, excellence, learning, creativity and compassion could really flourish. Due to the nature of co-operatives and the principles at their core, a powerful force could be released which provides alternative solutions for a more equitable society. styles, from John Lewis to Mondragon, or the model adopted by Jos de Blok in the Netherlands. But the reason I like it so much, is that it takes power from the few and shares it with the many. It allows for a different style of leadership and a different mode of making decisions. Collaborative conversations and compassionate care of one another in providing care to the wider community becomes the order of the day with leadership that is both clinical and managerial but modeled on financial benefits for everybody and cooperation of wider teams of people.
styles, from John Lewis to Mondragon, or the model adopted by Jos de Blok in the Netherlands. But the reason I like it so much, is that it takes power from the few and shares it with the many. It allows for a different style of leadership and a different mode of making decisions. Collaborative conversations and compassionate care of one another in providing care to the wider community becomes the order of the day with leadership that is both clinical and managerial but modeled on financial benefits for everybody and cooperation of wider teams of people. There are draw backs and co-operatives are not perfect, but they are a solution that should be seriously considered as General Practice tries to navigate itself into the future. They can be complex to set up, but I would argue that complexity is worth it when it offers a solution that lasts longer than a more straight forward quick-fix that may not make it past a decade or two. Are we brave enough to explore solutions that dis-empower us for the sake of a better future for everyone?
There are draw backs and co-operatives are not perfect, but they are a solution that should be seriously considered as General Practice tries to navigate itself into the future. They can be complex to set up, but I would argue that complexity is worth it when it offers a solution that lasts longer than a more straight forward quick-fix that may not make it past a decade or two. Are we brave enough to explore solutions that dis-empower us for the sake of a better future for everyone?