One of my favourite songs as a 5 year old was ‘Here We Go Round the Mulberry Bush’. I’ve been involved with the NHS for 17 years now and every winter, we do this same dance around Emergency Departments and the total mess that surrounds hospital admissions, discharges and an ever growing list of missed targets. Unfortunately, it no longer applies only to winter. It really is an absolute shambles and the problems are only too obvious. In this blog, I plan to outline them, but hopefully move away from the classic “who’s to blame” arguments and push through towards thinking about solutions…..none of which are easy, but neither are they rocket science!
So, here is a list of problems:
- We have an increasingly elderly population, who have increasingly complex health needs. You might not think this really means that much, but it has a profound impact on how long someone might need to stay in hospital and the kind of care they might require both in terms of social care and health care in the community. A recent report by the King’s Fund showed the extra strain on the health service due to a rise in people having multiple conditions is substantial. (http://www.kingsfund.org.uk/publications/pressures-in-general-practice)
- Funding cuts in social care and ‘efficiency savings’ in the NHS are having a terrible impact on hospitals and communities alike. If, as in our locality, wards have to be closed in order to balance the books, this has a massive knock on into several areas. If you close wards, it means the hospital fills up more quickly. If the hospital is full, then where do the patients who need to go into the hospital wait? The answer is in the ED. If they are waiting in the ED, then there becomes a back log of patients who cannot be seen and there will be an automatic failure to see, treat and admit or discharge patients within the 4 hour target window, which then leads to a negative rating for the hospital under CQC and pressure from on high to ‘do something about it’. But that’s just it….what can be done? Can people just be discharged home when they are unwell? – This is happening increasingly and then they end up back in hospital the next day in a worse state. The ED departments get the blame, but there is precious little they can do. At the other end of the line are people waiting to get home, but due to the deep cuts in social care, there simply isn’t the provision to put that care in place and so they are stuck. A lack of joined up computer systems between primary and secondary care makes this even more difficult. And even where patients could be cared for at home by community teams, the correct investment has not been made in this key area, hospital staff have not been trained to work in alternative environments (and believe me, they really are different) and so the teams we need in the community simply aren’t in place in many towns, cities and rural communities.
- There is a lack of information flow about patients and the care packages they already have in place and so a massive amount of time is wasted due to poor communication.
- The ‘A&E brand’ or ED, as it is now called is incredibly strong. Everybody knows it. And so people use it totally inappropriately, sometimes out of ignorance, sometimes desperation, sometimes laziness or convenience and sometimes apathy to the strain it places on services. We either have to work with this or keep on encouraging people not to use the ED. Unfortunately studies from the USA and Canada show that the more you negatively advertise the ED, the more people will use it. The King’s Fund explain with excellent clarity some of the complexities involved. What’s going on in A&E? The key questions answered (http://www.kingsfund.org.uk/projects/urgent-emergency-care/urgent-and-emergency-care-mythbusters?utm_source=twitter&utm_medium=social&utm_term=socialshare)
- Our residential and nursing home sector is in absolute disarray and in some areas of the country they are run like cartels, holding hospital trusts and county councils to ransom in terms of affordability.
- We are still unwilling to have a difficult and frank discussion about our attitude to death and how we often keep people alive for years, when we could allow them to die naturally and peacefully (I’ve blogged on this emotive subject previously).
So what happens is we have a circular blame culture in which everybody will blame somebody else, but nobody will take responsibility and so we will continue our dance around the mulberry bush! But if you have just a tiny bit of faith, you can say to this mulberry bush, “Be uprooted and be thrown into the Sea”. Where systems become oppressive and toxic, we must pluck up the complex root structure and find a new way.
Without real commitment from the government to invest rather than cut at this crucial time of transition, spending now to make huge savings in the long term, we might just continue this dance ad infinitum. The solutions cannot deliver change by the next parliament, but the transition must be honoured as vital and therefore allowed to happen over the next 10-20 years. We need a whole systems approach and it needs to involve the following (we’re trying this in Morecambe Bay):
Firstly, we need the development of Integrated Care Communities (ICCs). ICCs are geographically based, multidisciplinary teams, led and co-ordinated by a GP and a nurse but also include the vital mix of the fire service, police, mental health teams, social services, community matrons/long term conditions nurses, district nurses, community therapy teams and representatives of 3rd sector organisations. The idea of these teams to to keep care closer to home, share information, prevent admissions to hospital, but where admissions happen, ensure they happen in a coordinated way, bringing people back home as quickly as possible. We already have some great stories emerging here of this working really successfully. These teams have the potential to change the modus operandi and bring a culture change to how care is delivered.
However, these teams will fail for the same three key reasons the NHS is currently on the ropes. Resource, recruitment and IT.
These teams will be managing complex care in the community. With not too much extra funding, GPs and the care coordinators could do some incredibly effective work, but right now, general practice is at full stretch and so convincing community teams to take on this work will not be straight forward. This resource would be best invested in two areas – recruitment of staff, or retraining of staff and secondment of them from the hospital setting into the community and the strengthening of social care teams, (which to my mind are more accountable and more effective when under the same management as the NHS and provided by the state). The investment in it would also not be huge but it does involve some upfront cash. If each GP/Care Coordinator could have a laptop with Emis Web imbedded in it, with full access to their patients notes, they could go into the hospital setting once a week, do a ward round of their patients, who they know far better than the hospital teams and get them home. With the right team investment in the community this initiative would literally save millions of bed days and save an enormous amount of resource. But the better and more important benefit will be for patients themselves However, there is a warning for the government. In order for this to be effective and have the desired impact, it MUST be double-run, rather than expecting this to be done on top of what is already the status quo. The capacity is simply not in the system, but it could so easily be and this could be utterly transformational.
Secondly, the government must reverse the perverse cuts to funding. It simply bad mathematics to think that you can shrink the size of a hospital and shrink the social care provision available in the community at the same time. We need a serious reinvestment in social care. A strong and well paid social sector will bring more people into work, which btw builds a stronger economy.
Thirdly, we need to ensure all people in residential and nursing care, and those living with complex health conditions in the community have detailed care plans in place to avoid hospital admissions, except when absolutely necessary AND in line with the persons own wishes.
Fourthly, we must co-create urgent care strategies, not designed from on high, but collaboratively between ED departments, mental health teams, the police, GPs, community nursing teams and social services. If we cannot undo fifty years of public mindset about the ED, then let’s work with this rather than against it. We need more people recruited to work in the emergency setting and the pay needs to reflect the complexity and unsocial nature of the work.
Fifthly, we must stop the nonsense around data sharing, make patient records available to patients themselves and front end our EDs, Acute Medical and Surgical Units, Outpatient Departments with the same systems as we find in the GPs, all of whom should agree to share their records. In our area this would be with Emis Web, a very straight forward system to use. It would mean far faster diagnostics, more joined up, effective care for patients and investment now by the government across the UK would save them plenty of money within just a few years. It would also make data gathering, audit and governance easier and safer. The idea of spending literally millions of pounds on apps that can input data straight into patients notes, before we have this far more vital infrastructure in place is quite frankly ridiculous!
Lastly, we must work creatively with communities on public health strategies that can have a lasting impact and so stave off the growing health crises we see emerging for the future.
I don’t know about you, but to me the dance around this mulberry bush has become pretty boring, a colossal waste of time and energy and so in my opinion, we should quite simply stop it and do something different. The solutions are right in front of us. Will the government have the guts to stop what they are doing and make the right investments now for the sake of the health and wellbeing of the population at large and the health and social care system as a whole. They might not get the glory at the next election, but in ten years time, we will see that the right choices were made for the good of all.
 We’ve got a problem (well 4 actually), when it comes to medical education! The first is this: Jeremy Hunt is promising loads of new places at medical school – I know this doesn’t sound like a problem, it sounds like a solution. But the truth is, once you actually do some number crunching, the new places won’t even account for the losses we will have due to retirement over the next 10 years, let alone account for the increased need there is in the system. So…..we’re still going to be short of doctors. Unfortunately – there isn’t a political appetite to increase these numbers further, and with our exit from the EU we’re genuinely facing an ongoing crisis.
We’ve got a problem (well 4 actually), when it comes to medical education! The first is this: Jeremy Hunt is promising loads of new places at medical school – I know this doesn’t sound like a problem, it sounds like a solution. But the truth is, once you actually do some number crunching, the new places won’t even account for the losses we will have due to retirement over the next 10 years, let alone account for the increased need there is in the system. So…..we’re still going to be short of doctors. Unfortunately – there isn’t a political appetite to increase these numbers further, and with our exit from the EU we’re genuinely facing an ongoing crisis. creative way, to work more smartly and differently, with a flexible workforce, but due to the pressures upon the system, there is little room for people to put much time or imagination into this and there is also a huge leap of faith involved. There is simply not the evidence base in place to support the leap we are asking GPs, in particular, to take in restructuring their practices and not replace GPs with GPs, but with combinations of paramedics, advanced practitioners, physician assistants, physics, mental health workers, health coaches and the like. However, the issue is that the system finds itself, like Indiana Jones, at the edge of a cliff, with no way back and the only thing for it is to step into the unknown and hope that God supplies the stepping stones…..Those in leadership positions are going to have be given space and grace to try some things, get it wrong and try again……One of the vital things that will be involved is proper engagement with the communities we serve. Clinicians and the general population need to have a better and deeper understanding of one another. There is a huge language void to be bridged and a collaboration that is needed in understanding how services can be more helpfully redesigned for the benefit of everybody. It also means where there are are difficult decisions to be made, there are no cloak and daggers or suspicion, but honest, open communication in the light of day that builds trust and partnership.
creative way, to work more smartly and differently, with a flexible workforce, but due to the pressures upon the system, there is little room for people to put much time or imagination into this and there is also a huge leap of faith involved. There is simply not the evidence base in place to support the leap we are asking GPs, in particular, to take in restructuring their practices and not replace GPs with GPs, but with combinations of paramedics, advanced practitioners, physician assistants, physics, mental health workers, health coaches and the like. However, the issue is that the system finds itself, like Indiana Jones, at the edge of a cliff, with no way back and the only thing for it is to step into the unknown and hope that God supplies the stepping stones…..Those in leadership positions are going to have be given space and grace to try some things, get it wrong and try again……One of the vital things that will be involved is proper engagement with the communities we serve. Clinicians and the general population need to have a better and deeper understanding of one another. There is a huge language void to be bridged and a collaboration that is needed in understanding how services can be more helpfully redesigned for the benefit of everybody. It also means where there are are difficult decisions to be made, there are no cloak and daggers or suspicion, but honest, open communication in the light of day that builds trust and partnership. Fourthly, our medical schools are delivering a curriculum, designed centrally but based on yesterdays NHS. There is not enough creative vision around the curriculum to build the right kind of future doctors. There is still far too much focus on illness and disease and no where near enough thought or teaching about wellness, healthy lifestyles, nutrition and non-pharmacological options. The role of the future doctor is much more population focused and digitally savvy. It is our medical schools more than anywhere else that carry the responsibility to ensure the future NHS is catered for. We need a radical shake up in medical education and some brave people to rewrite the curriculum that will enable medical schools to be more creative and engaging in helping to raise the doctors we need for the future.
Fourthly, our medical schools are delivering a curriculum, designed centrally but based on yesterdays NHS. There is not enough creative vision around the curriculum to build the right kind of future doctors. There is still far too much focus on illness and disease and no where near enough thought or teaching about wellness, healthy lifestyles, nutrition and non-pharmacological options. The role of the future doctor is much more population focused and digitally savvy. It is our medical schools more than anywhere else that carry the responsibility to ensure the future NHS is catered for. We need a radical shake up in medical education and some brave people to rewrite the curriculum that will enable medical schools to be more creative and engaging in helping to raise the doctors we need for the future. feeling low/down/hopeless/sad/apathetic/bored/exhausted, I might invite you to imagine what life might be like if you weren’t feeling that way. You might tell me that you’d feel happy and then I would ask you to tell me what ‘happiness’ might be like for you. I’d ask you to describe in as much detail as possible how you would know that you were happy – what would be different? I’d get you to put as much colour on that as possible. And once I understood how you would know you were happy, I would ask how others around you would know – what your partner/children/friends/pets would notice about you…….suddenly your mind is alive with an alternative reality to where you are currently and although things won’t be suddenly better, your mind has been awakened to another way of being! And that brings a beautiful thing – it brings possible solutions to the problem.
feeling low/down/hopeless/sad/apathetic/bored/exhausted, I might invite you to imagine what life might be like if you weren’t feeling that way. You might tell me that you’d feel happy and then I would ask you to tell me what ‘happiness’ might be like for you. I’d ask you to describe in as much detail as possible how you would know that you were happy – what would be different? I’d get you to put as much colour on that as possible. And once I understood how you would know you were happy, I would ask how others around you would know – what your partner/children/friends/pets would notice about you…….suddenly your mind is alive with an alternative reality to where you are currently and although things won’t be suddenly better, your mind has been awakened to another way of being! And that brings a beautiful thing – it brings possible solutions to the problem. There is no doubting that the problems in the NHS are vast. One of the things I have found is that if you try and enable someone to think about the solutions without allowing them to tel you what the problems are, you won’t get very far. A certain amount of catharsis and expression of the issues is important. So here goes: here is a picture of the problems the NHS faces (and these have already been stated many times over, but let’s just be clear):
There is no doubting that the problems in the NHS are vast. One of the things I have found is that if you try and enable someone to think about the solutions without allowing them to tel you what the problems are, you won’t get very far. A certain amount of catharsis and expression of the issues is important. So here goes: here is a picture of the problems the NHS faces (and these have already been stated many times over, but let’s just be clear): The NHS is under-funded. Cuts to other services, like social care have also had a massive impact on the NHS as a system being able to work and targets are being missed as a result. People are living longer and this means more complex health problems and a rise in dementia. There is more obesity and diabetes and this has a huge impact in the cost of healthcare. The way the NHS is funded is ludicrous and puts parts of the system that should be working collaboratively in direct competition with each other. Teams across the NHS are clumsy and clunky with little ability to work smartly due to constraints of historic ways things were set up. Demand and expectation are extremely high and yet there are multiple missed appointments. And I could go on!
The NHS is under-funded. Cuts to other services, like social care have also had a massive impact on the NHS as a system being able to work and targets are being missed as a result. People are living longer and this means more complex health problems and a rise in dementia. There is more obesity and diabetes and this has a huge impact in the cost of healthcare. The way the NHS is funded is ludicrous and puts parts of the system that should be working collaboratively in direct competition with each other. Teams across the NHS are clumsy and clunky with little ability to work smartly due to constraints of historic ways things were set up. Demand and expectation are extremely high and yet there are multiple missed appointments. And I could go on! eat moany pie together and complain about the issues. Throwing mud and finger pointing, blaming everybody else but ourselves will solve nothing. The awful tribalism and over politicization of the NHS is preventing us from finding a way forward. What might health and social care in this country be like if open our mind to new possibilities? What if we stopped focusing on all the problems and dreamed of how things might be in 5, 10, 50, 100 years time? We’ve been doing this in Morecambe Bay and we’re moving from not only dreaming but to doing something different!
eat moany pie together and complain about the issues. Throwing mud and finger pointing, blaming everybody else but ourselves will solve nothing. The awful tribalism and over politicization of the NHS is preventing us from finding a way forward. What might health and social care in this country be like if open our mind to new possibilities? What if we stopped focusing on all the problems and dreamed of how things might be in 5, 10, 50, 100 years time? We’ve been doing this in Morecambe Bay and we’re moving from not only dreaming but to doing something different! We’re working with our communities to help us all live more healthy lives, thinking about health as a social movement. 97% of all health monies are spent once people are ill. We’re taking prevention seriously! We are breaking down walls between our organisations and sharing our budgets. We’re building relationships between clinicians and managers across many diving lines. We’re collaborating to share our resources and using our budgets in a way that makes sense for our communities. We’re unashamedly talking a new language of love, building trust and establishing infrastructures of positive peace. We’ve worked out where we are being inefficient and sharing our conundrums with our communities (we do actually have to be responsible about what we spend – the NHS is not carte blanche). We’re working out how to work differently and more smartly. We’re sorting out our IT. We’re redesigning care so it makes more sense for our patients. We’re working on our consultation and communication skills. We’re being more proactive in getting positive messages out there. We’re building for the next 100+ years not just the next political cycle. This is better care together!
We’re working with our communities to help us all live more healthy lives, thinking about health as a social movement. 97% of all health monies are spent once people are ill. We’re taking prevention seriously! We are breaking down walls between our organisations and sharing our budgets. We’re building relationships between clinicians and managers across many diving lines. We’re collaborating to share our resources and using our budgets in a way that makes sense for our communities. We’re unashamedly talking a new language of love, building trust and establishing infrastructures of positive peace. We’ve worked out where we are being inefficient and sharing our conundrums with our communities (we do actually have to be responsible about what we spend – the NHS is not carte blanche). We’re working out how to work differently and more smartly. We’re sorting out our IT. We’re redesigning care so it makes more sense for our patients. We’re working on our consultation and communication skills. We’re being more proactive in getting positive messages out there. We’re building for the next 100+ years not just the next political cycle. This is better care together!
 have huge health inequalities. There are major issues with housing, economic policies that are not working for huge swathes of our population, with more people having to use food banks, struggling with fuel poverty, living in damp houses and unable to make ends meet. Yes, our kids are spending more time on screens and less time in activity. Yes, the sugar lobby, alcohol lobby and advertising giants have far too much power. Supermarkets are designed deliberately so that we buy things that are bad for us. And sometimes, we just make poor choices (if you can call them choices, which for some people, they aren’t always) – we do not all live as healthily as we could – we eat the wrong stuff, work highly stressful jobs, and exercise less than we are recommended to. Mental health issues are on the rise, especially for teenagers, due to crazy targets and league tables, with all the pressures they face. We are less happy and more separated than we ever used to be, despite the rise in social media…..(or maybe because of it……)…..Man, I can paint a negative picture – it’s like storm clouds and darkness everywhere……..
have huge health inequalities. There are major issues with housing, economic policies that are not working for huge swathes of our population, with more people having to use food banks, struggling with fuel poverty, living in damp houses and unable to make ends meet. Yes, our kids are spending more time on screens and less time in activity. Yes, the sugar lobby, alcohol lobby and advertising giants have far too much power. Supermarkets are designed deliberately so that we buy things that are bad for us. And sometimes, we just make poor choices (if you can call them choices, which for some people, they aren’t always) – we do not all live as healthily as we could – we eat the wrong stuff, work highly stressful jobs, and exercise less than we are recommended to. Mental health issues are on the rise, especially for teenagers, due to crazy targets and league tables, with all the pressures they face. We are less happy and more separated than we ever used to be, despite the rise in social media…..(or maybe because of it……)…..Man, I can paint a negative picture – it’s like storm clouds and darkness everywhere…….. But what if it wasn’t that way? What if we got a bit angry about it, but instead of finding someone to blame and pointing the finger; instead of getting all tribal and throwing stones at others, we chose to use our energies creatively to find solutions, to work together and make positive changes?! Let’s put away our pointing fingers and our ranting tongues and let’s work together for a better future for everyone! Doesn’t that sound good?! It’s what we’re trying here in Morecambe Bay, and I’m hoping it spreads like wild fire so that we can become a place where health abounds and beauty surrounds (that’s the motto of this place!). That doesn’t mean we stop speaking truth to power, but we also let our actions (and maybe our votes) speak louder than ever before.
But what if it wasn’t that way? What if we got a bit angry about it, but instead of finding someone to blame and pointing the finger; instead of getting all tribal and throwing stones at others, we chose to use our energies creatively to find solutions, to work together and make positive changes?! Let’s put away our pointing fingers and our ranting tongues and let’s work together for a better future for everyone! Doesn’t that sound good?! It’s what we’re trying here in Morecambe Bay, and I’m hoping it spreads like wild fire so that we can become a place where health abounds and beauty surrounds (that’s the motto of this place!). That doesn’t mean we stop speaking truth to power, but we also let our actions (and maybe our votes) speak louder than ever before. We’re talking together, taking time to dream about what it would be like if we were the healthiest area in the UK. We’re training up many people to host conversations, so that we break down walls and learn to collaborate for the sake of everyone. We’re not just dreaming about physical health, but mental, social and systemic health as well. We’re encouraging those who want to rise up and take some leadership, to be pioneers in the stuff they are passionate about. Even in my little town, we now have a mental health cafe that is literally saving people’s lives, because a lady called Jane wanted to make a difference. We have a cafe for all the people who have circulation problems because one of our nurses wanted to break people’s isolation and improve their healing rates at the same time.
We’re talking together, taking time to dream about what it would be like if we were the healthiest area in the UK. We’re training up many people to host conversations, so that we break down walls and learn to collaborate for the sake of everyone. We’re not just dreaming about physical health, but mental, social and systemic health as well. We’re encouraging those who want to rise up and take some leadership, to be pioneers in the stuff they are passionate about. Even in my little town, we now have a mental health cafe that is literally saving people’s lives, because a lady called Jane wanted to make a difference. We have a cafe for all the people who have circulation problems because one of our nurses wanted to break people’s isolation and improve their healing rates at the same time.  We’ve got a carers cafe, a dementia cafe and will soon have a breathing cafe for those who have severe COPD, sharing ideas and diminishing anxiety. We’ve got exercise classes to help with pain, a community choir, dog poo wardens to help us take more pride when we walk down the street and food banks to help those who can no longer afford to eat.
We’ve got a carers cafe, a dementia cafe and will soon have a breathing cafe for those who have severe COPD, sharing ideas and diminishing anxiety. We’ve got exercise classes to help with pain, a community choir, dog poo wardens to help us take more pride when we walk down the street and food banks to help those who can no longer afford to eat.![image[1]](http://reimagininghealth.com/wp-content/uploads/2016/03/image1.jpg) We have 2000 kids aged 4-11 running a mile a day at school with staggering results for our children here in terms of physical, mental and educational health. We’re hoping over time, this becomes the Morecambe Bay Mile, part of a cultural shift towards being more active. We are working with local chefs and supermarkets to enable people with pre-diabetes or weight struggles to eat more healthily. We’re choosing to lead by example in the NHS to work well and flourish in our work places. We’ve made a commitment to see the 5 ways to wellbeing in every NHS organisation and we’re hoping many other systems and businesses will follow us in this. We’re finding radical ways to help people who are struggling with alcohol and drug addiction, get free and stay free with amazing results. We’re helping people live well with and beyond cancer.
We have 2000 kids aged 4-11 running a mile a day at school with staggering results for our children here in terms of physical, mental and educational health. We’re hoping over time, this becomes the Morecambe Bay Mile, part of a cultural shift towards being more active. We are working with local chefs and supermarkets to enable people with pre-diabetes or weight struggles to eat more healthily. We’re choosing to lead by example in the NHS to work well and flourish in our work places. We’ve made a commitment to see the 5 ways to wellbeing in every NHS organisation and we’re hoping many other systems and businesses will follow us in this. We’re finding radical ways to help people who are struggling with alcohol and drug addiction, get free and stay free with amazing results. We’re helping people live well with and beyond cancer.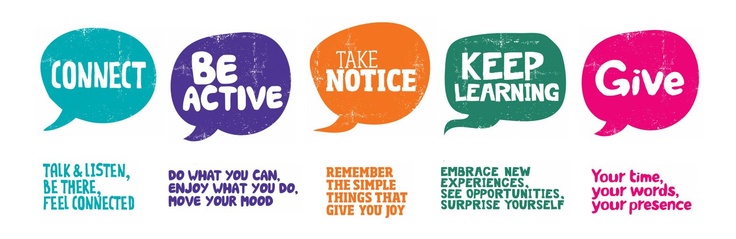 We’re changing the way consultations happen in the NHS to enable people to make more informed and better choices about their own health and conditions, so they feel empowered to make changes that work for them rather than beaten up when they go for an appointment! We’re launching the Morecambe Bay Poverty Truth challenge, learning from those who are lived
We’re changing the way consultations happen in the NHS to enable people to make more informed and better choices about their own health and conditions, so they feel empowered to make changes that work for them rather than beaten up when they go for an appointment! We’re launching the Morecambe Bay Poverty Truth challenge, learning from those who are lived  experts in poverty to help us work together and care better for those most struggling in our society. We’re having difficult conversations about death to help people be prepared for every eventuality.
experts in poverty to help us work together and care better for those most struggling in our society. We’re having difficult conversations about death to help people be prepared for every eventuality. will be awakened? What other partnerships, collaborations and relationships might be formed? Being all tribal and accusatory of others saps our energy and stops us being creative. Mud slinging and blame will achieve little. We have to work from where we are. We have to build bridges and work together. We have to build a future of positive peace and that means binary thinking is over! The future doesn’t have to be full of doom and gloom. It is alive with hope! What resources might we find? What talents might we discover? What might we see develop over the next 12 months/years/decades as we look for solutions together for a better future for everybody? Don’t you feel just a little bit excited?
will be awakened? What other partnerships, collaborations and relationships might be formed? Being all tribal and accusatory of others saps our energy and stops us being creative. Mud slinging and blame will achieve little. We have to work from where we are. We have to build bridges and work together. We have to build a future of positive peace and that means binary thinking is over! The future doesn’t have to be full of doom and gloom. It is alive with hope! What resources might we find? What talents might we discover? What might we see develop over the next 12 months/years/decades as we look for solutions together for a better future for everybody? Don’t you feel just a little bit excited?

![1973049_861ba277[1]](http://reimagininghealth.com/wp-content/uploads/2016/03/1973049_861ba2771.jpg)