Here in Morecambe Bay, we are trying to develop a strategy around Population Health – by that we mean we want to take a much broader view of the health needs of those who live in this area, ensuring that we try to tackle the disparities we see in the health of our population. In my opinion this needs a three fold approach.
Firstly, we need to get our own house in order. We know there is work

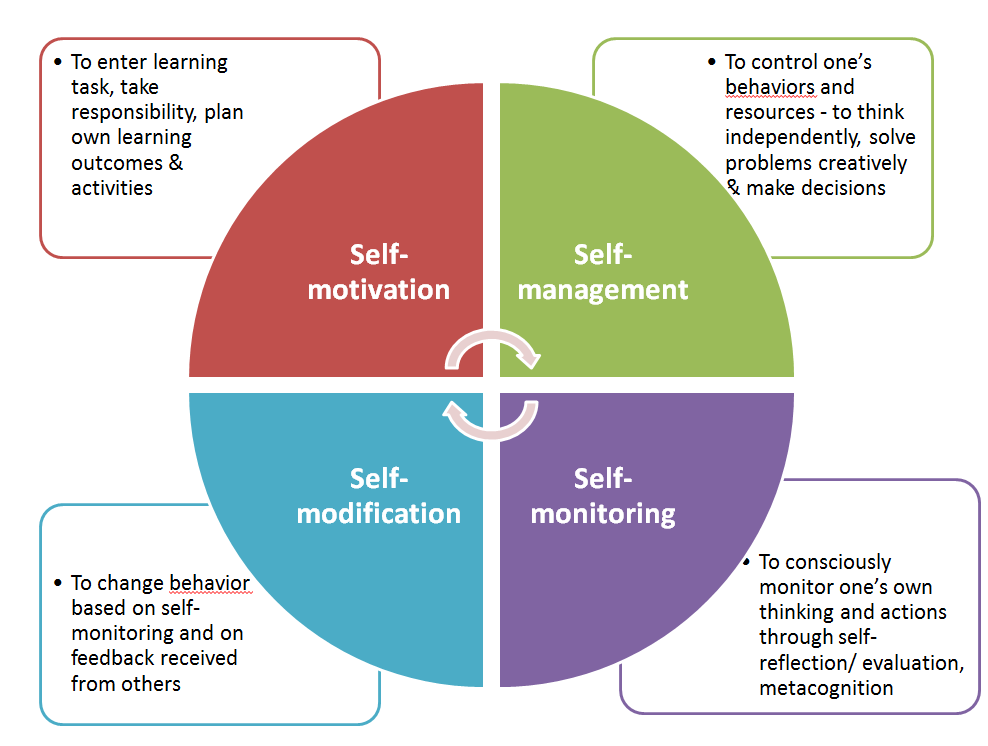
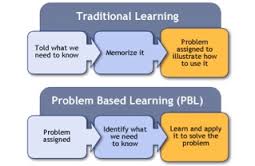
for us to do as a health system when it comes to ensuring we’re proactive with people’s health. With the resources we have available, we need to ensure that we are treating preventable conditions as well as possible and use the best evidenced-based approach to the care we are delivering. That is why, the excellent Medical Director of UHMB, Dr David Walker, with his vast experiencing in Public Health, is helping us focus on making a significant difference to preventing Strokes (CVAs – Cerebro-Vascular Accidents) across the Bay this year. We are making a concerted effort to ensure that all our patients are getting the necessary pulse checks, blood pressure checks, blood tests and appropriate medications to monitor and manage conditions which can lead to devastating consequences if left untreated or mismanaged. Within this, we are encouraging people to know more about the conditions they live with, understand them and take responsibility to ensure that they are caring for their own health.
 Secondly, we are working with people across the Bay to live more healthy lives. We continue to see more and more children running a mile a day and hope that this will soon become the Morecambe Bay Mile, in which it becomes the norm for everyone who lives here to move a mile a day. Our sedentary lifestyles are hugely affecting our health and we’re wanting to encourage all business owners and leaders to ensure that staff have time to be active every day. On top of this we’re starting to work with schools around healthy eating and involved in projects with supermarkets to enable people to make more healthy choices in the face of fierce advertising. We’re also working with high schools around mental health issues and seeing many community initiatives springing up, run by the community for the community, which will improve the wellbeing of all. All of this is backed by our ‘Flourish’ work in our hospitals and ‘Let’s Work Well’ in the community, in which NHS staff are leading by example in changing the way that we work and live.
Secondly, we are working with people across the Bay to live more healthy lives. We continue to see more and more children running a mile a day and hope that this will soon become the Morecambe Bay Mile, in which it becomes the norm for everyone who lives here to move a mile a day. Our sedentary lifestyles are hugely affecting our health and we’re wanting to encourage all business owners and leaders to ensure that staff have time to be active every day. On top of this we’re starting to work with schools around healthy eating and involved in projects with supermarkets to enable people to make more healthy choices in the face of fierce advertising. We’re also working with high schools around mental health issues and seeing many community initiatives springing up, run by the community for the community, which will improve the wellbeing of all. All of this is backed by our ‘Flourish’ work in our hospitals and ‘Let’s Work Well’ in the community, in which NHS staff are leading by example in changing the way that we work and live.
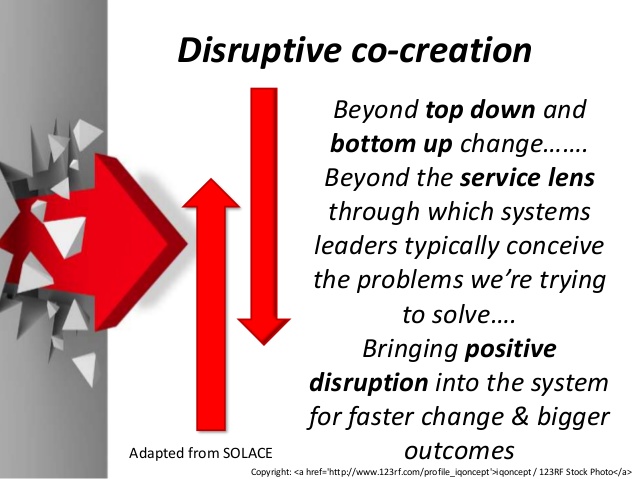
 Thirdly, however, we need to dig deeper. We keep trying to put a sticky plaster over the great pus-filled abscesses that are the leading causes of ill health in our country. Traditionally we have paid much of our attention to dealing with the symptoms of ill health, and whilst thinking about the root causes, we have simply not putting anyway near enough time, energy, or resource into tackling them. The reason for this is two fold: firstly, health and social policy is directed far too much by the political cycle and the short term gains that can proven in small time windows – so we keep tackling symptoms because we can then prove how effective we are!; secondly, in truth, we don’t actually know how to tackle some of the issues and those of us in leadership roles are far too clever and proud to admit that we don’t know how to fix them and that we need to find a new way together, with the communities of which we are a part.
Thirdly, however, we need to dig deeper. We keep trying to put a sticky plaster over the great pus-filled abscesses that are the leading causes of ill health in our country. Traditionally we have paid much of our attention to dealing with the symptoms of ill health, and whilst thinking about the root causes, we have simply not putting anyway near enough time, energy, or resource into tackling them. The reason for this is two fold: firstly, health and social policy is directed far too much by the political cycle and the short term gains that can proven in small time windows – so we keep tackling symptoms because we can then prove how effective we are!; secondly, in truth, we don’t actually know how to tackle some of the issues and those of us in leadership roles are far too clever and proud to admit that we don’t know how to fix them and that we need to find a new way together, with the communities of which we are a part.
 I was having a conversation with Cormac Russell the other day, via twitter, and he gave me this beautiful quote by Ivan Illich: “I believe it is time to state clearly that specific situations and circumstances are “sickening”, rather than that people themselves are sick. The symptoms which modern medicine attempts to treat often have little to do with the condition of our bodies; they are, rather, signals pointing to the disorders and presumptions of modern ways of working, playing and living.”
I was having a conversation with Cormac Russell the other day, via twitter, and he gave me this beautiful quote by Ivan Illich: “I believe it is time to state clearly that specific situations and circumstances are “sickening”, rather than that people themselves are sick. The symptoms which modern medicine attempts to treat often have little to do with the condition of our bodies; they are, rather, signals pointing to the disorders and presumptions of modern ways of working, playing and living.”
 The reality is that many of the determinants of our health and especially of the health inequalities we see in our society have little to do with the availability or quality of services. No, the biggest factors affecting the health gap in this (and every) area are poverty, housing, loneliness, hopelessness and adverse childhood experiences. If we’re not careful, we end up thinking the real issues are waiting times in the ED, difficulties discharging people from hospital, breaking the 18 week target for hip and knee operations and ensuring there are enough GP appointments at weekends. We must not look at the symptoms and believe that if we tackle these surface issues then we will automatically have better health outcomes for all. Here in the Bay, we are trying to be brave enough to take off the sticky plaster and gaze into the festering wounds in our society, so that we can begin to really do some deep debridement of them and allow real healing to ensue.
The reality is that many of the determinants of our health and especially of the health inequalities we see in our society have little to do with the availability or quality of services. No, the biggest factors affecting the health gap in this (and every) area are poverty, housing, loneliness, hopelessness and adverse childhood experiences. If we’re not careful, we end up thinking the real issues are waiting times in the ED, difficulties discharging people from hospital, breaking the 18 week target for hip and knee operations and ensuring there are enough GP appointments at weekends. We must not look at the symptoms and believe that if we tackle these surface issues then we will automatically have better health outcomes for all. Here in the Bay, we are trying to be brave enough to take off the sticky plaster and gaze into the festering wounds in our society, so that we can begin to really do some deep debridement of them and allow real healing to ensue.
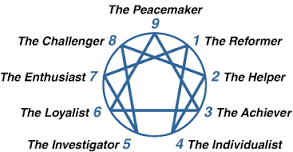
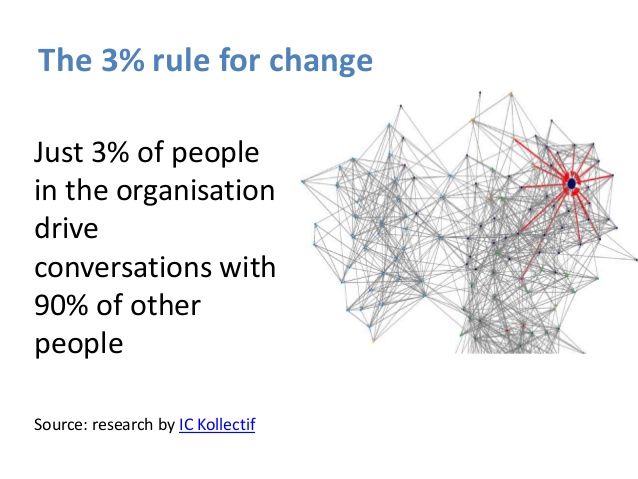
That is why my team are focusing on hosting conversations that matter across our communities and seeking to co-create a social movement. Using the ‘Art of Hosting’ we are holding spaces open in which rich conversations can happen. “We don’t just want people to be more healthy and well – many people don’t even know what that means”, as an amazing woman called Gill, from the West End of Morecambe told us recently, “No, we want everyone to be able to experience life to the full, whatever that means for them”. We can’t do this simply by having good clinical strategies – we need something far more holistic and it will involve all of us. We need to start our conversations together with appreciative inquiry. What is already going well? What can we learn from here? Knowing what is good, however, is not enough – we must go further, dig deeper and get to grips with some extremely difficult issues.
 When it comes to Poverty, here in Morecambe Bay, we are trying out new economies (like time banking) and having challenging conversations. The Poverty Truth Commission is causing is to really listen to those with lived experience of poverty and learn to co-create and co-commission services, rather than presuming that the ‘experts’ know best.
When it comes to Poverty, here in Morecambe Bay, we are trying out new economies (like time banking) and having challenging conversations. The Poverty Truth Commission is causing is to really listen to those with lived experience of poverty and learn to co-create and co-commission services, rather than presuming that the ‘experts’ know best.
 When it comes to homelessness, inspired by the work in Alberta Canada (https://www.goodnewsnetwork.org/find-out-how-this-canadian-city-has-eliminated-homelessness/) and the Manchester Homelessness Charter (https://charter.streetsupport.net/) – we’re beginning to explore ‘housing first’ for Morecambe Bay, but imagining what it might be like with extra support in place from a caring community like ‘The Well’ in Morecambe and Barrow (https://www.thewellcommunities.co.uk/). I’m so pleased that Dave Higham is provoking this conversation for us here and I’m excited to see where a conversation between those with lived experience of homelessness, poverty and addiction, along with some of us in the public sector, might take us. There’s a challenge to all of us in society – we like the sound of these kind of things, but not in our own backyard….our values must begin to align with our actions. Love without action is not really love.
When it comes to homelessness, inspired by the work in Alberta Canada (https://www.goodnewsnetwork.org/find-out-how-this-canadian-city-has-eliminated-homelessness/) and the Manchester Homelessness Charter (https://charter.streetsupport.net/) – we’re beginning to explore ‘housing first’ for Morecambe Bay, but imagining what it might be like with extra support in place from a caring community like ‘The Well’ in Morecambe and Barrow (https://www.thewellcommunities.co.uk/). I’m so pleased that Dave Higham is provoking this conversation for us here and I’m excited to see where a conversation between those with lived experience of homelessness, poverty and addiction, along with some of us in the public sector, might take us. There’s a challenge to all of us in society – we like the sound of these kind of things, but not in our own backyard….our values must begin to align with our actions. Love without action is not really love.
 And what about loneliness and hopelessness? More than ever, we need connection across the generations, turning off our screens and actually being together as humans. In Morecambe we are seeing the launch of the new Morecambe Fringe in September, bringing people together around Comedy and the Arts. More Music are doing incredible work with young people. There are amazing community initiatives right around the Bay. We have loads of festivals connecting people across the district. And what is the role of business here? We need businesses to think abut what kind of enterprise we could see emerge for the youth in our area. Are there more opportunities for mentoring? We have left many of our young people to boredom and with few aspirations. With the help of Stanley’s Youth Centre and the great heart of Yak Patel, we hope to host many conversations with young people to really listen to what it is we could create together to break these problems and build community and hope.
And what about loneliness and hopelessness? More than ever, we need connection across the generations, turning off our screens and actually being together as humans. In Morecambe we are seeing the launch of the new Morecambe Fringe in September, bringing people together around Comedy and the Arts. More Music are doing incredible work with young people. There are amazing community initiatives right around the Bay. We have loads of festivals connecting people across the district. And what is the role of business here? We need businesses to think abut what kind of enterprise we could see emerge for the youth in our area. Are there more opportunities for mentoring? We have left many of our young people to boredom and with few aspirations. With the help of Stanley’s Youth Centre and the great heart of Yak Patel, we hope to host many conversations with young people to really listen to what it is we could create together to break these problems and build community and hope.
 What are we together going to do about the huge issue that is child abuse? We don’t have answers, but we do have questions – and we need to keep asking them. We know that the mental and physical consequences of abuse are utterly devastating and we find it hard to talk about because it affects so many of us. But our interventions are happening too little, too late, and we are missing the vast majority of cases. Our services simply cannot cope with the volume and serious case reviews tell us the same lessons nearly every time. So what? What are we going to do differently? There are definitely things that the public services can do better – but not when our resources are being stripped. What is especially terrible about the cuts to services in our most deprived areas is that ACEs cause poverty, homelessness, isolation and ill health! As a team, we take this really seriously and will be hosting discussions in our schools and local communities about how we raise happy, healthy children. Where is help needed? We’ve become so focused on grades and outcomes in schools…..but do we teach people what to do with their anger? Do we focus enough on values? Are there enough parenting (the hardest job in the world) classes – and if so, are they hitting the mark? What do we need to do differently? We know the situations in which children are more likely to suffer – so what? Have we become so focused on getting people into work that we’ve forgotten just how important parenting is? And if we know that ACE is such a massive issue, are we really making the right choices in terms of what therapies we’re making available for those who have suffered them?
What are we together going to do about the huge issue that is child abuse? We don’t have answers, but we do have questions – and we need to keep asking them. We know that the mental and physical consequences of abuse are utterly devastating and we find it hard to talk about because it affects so many of us. But our interventions are happening too little, too late, and we are missing the vast majority of cases. Our services simply cannot cope with the volume and serious case reviews tell us the same lessons nearly every time. So what? What are we going to do differently? There are definitely things that the public services can do better – but not when our resources are being stripped. What is especially terrible about the cuts to services in our most deprived areas is that ACEs cause poverty, homelessness, isolation and ill health! As a team, we take this really seriously and will be hosting discussions in our schools and local communities about how we raise happy, healthy children. Where is help needed? We’ve become so focused on grades and outcomes in schools…..but do we teach people what to do with their anger? Do we focus enough on values? Are there enough parenting (the hardest job in the world) classes – and if so, are they hitting the mark? What do we need to do differently? We know the situations in which children are more likely to suffer – so what? Have we become so focused on getting people into work that we’ve forgotten just how important parenting is? And if we know that ACE is such a massive issue, are we really making the right choices in terms of what therapies we’re making available for those who have suffered them?
Is it the role of those of us in healthcare to get involved in these discussions? YES! It is the role of all of us in society. Together, we must reimagine the future. We all know that prevention is better than cure, but our short-termism is stopping us from finding the kind of positive solutions that will really make a difference. In face of downward pressure from hierarchical powers, it is tough to make brave decisions to invest in the future, rather than cut our way to balancing the books. But if we really care about the health and wellbeing of our communities, then we have to stop the sticking plaster approach and clean out the gangrenous wounds in our society. We have to deal with the root and not the fruit.
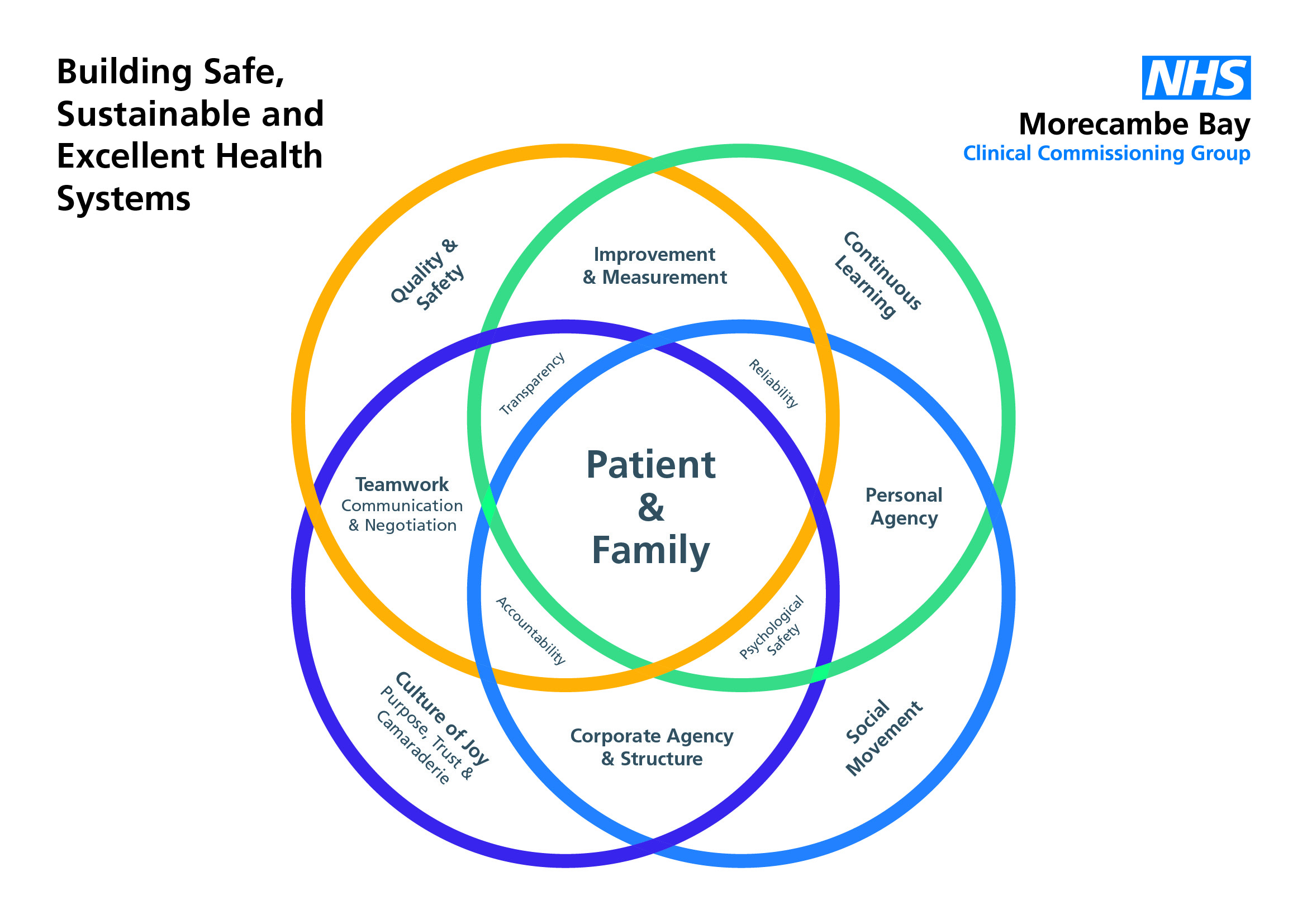



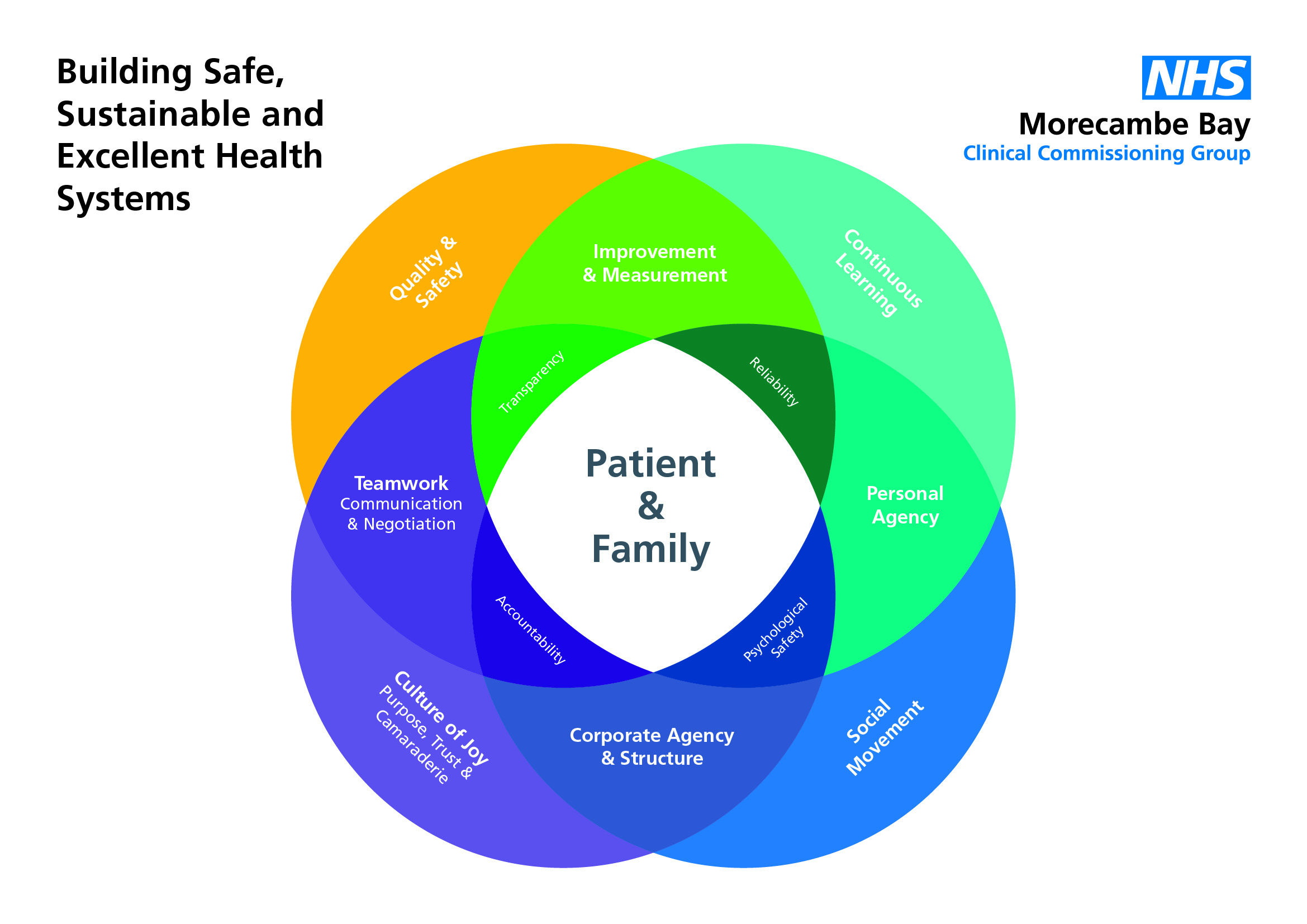





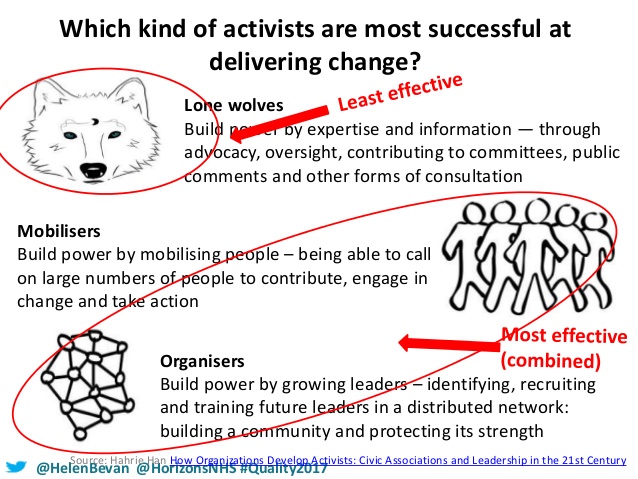

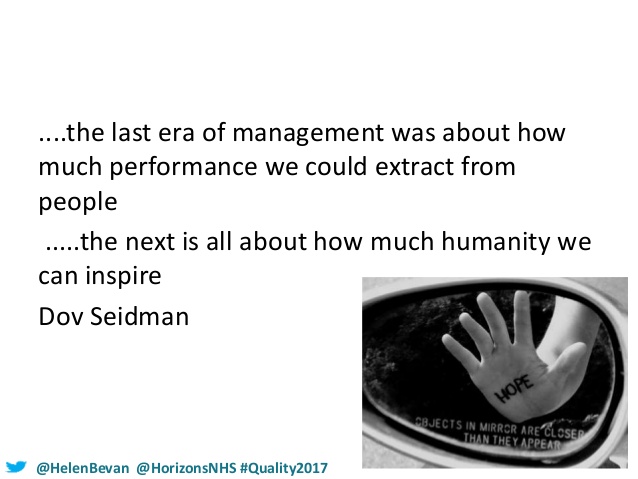



 In my last blog, I talked about the exponential potential of what could be possible if clinicians worked together in a more collaborative way. However, far more can be achieved if we work together in and with our communities to create a social movement together around being more healthy and well. I’ve talked previously about the “battle royale” that occurred between Béchamp and Pasteur over whether we should promote health or fight disease. The answer is, of course, that we need to do both, but the clinical community is not equipped with the resource or power to do it alone.
In my last blog, I talked about the exponential potential of what could be possible if clinicians worked together in a more collaborative way. However, far more can be achieved if we work together in and with our communities to create a social movement together around being more healthy and well. I’ve talked previously about the “battle royale” that occurred between Béchamp and Pasteur over whether we should promote health or fight disease. The answer is, of course, that we need to do both, but the clinical community is not equipped with the resource or power to do it alone. crises we now face are too much for us to do anything about. We are in the midst of a battle, which we are currently losing and it is time to gird our loins for a turning of the tide. Here in Morecambe Bay, we have started a conversation, not just among the Clinical Community but with the wider population about how we might become the healthiest place in the UK. Yes, we mean this in a very holistic way, but there are also some specific foci we have so we can together reverse some of the appalling health statistics we are facing.
crises we now face are too much for us to do anything about. We are in the midst of a battle, which we are currently losing and it is time to gird our loins for a turning of the tide. Here in Morecambe Bay, we have started a conversation, not just among the Clinical Community but with the wider population about how we might become the healthiest place in the UK. Yes, we mean this in a very holistic way, but there are also some specific foci we have so we can together reverse some of the appalling health statistics we are facing. I suggest that within a generation, if we wanted to, we could render Type 2 Diabetes a rare diagnosis. We can do this through encouraging far more healthy lifestyles in our children and young people now, like running a mile a day and learning to eat food that doesn’t actually harm them! I believe we could significantly reduce the need for so many people to be taking medication for hypertension and diabetes now, prevent many strokes and heart attacks, by being violent towards these conditions with major changes in lifestyle, though diet and exercise, rather than the prescription of drugs, using coaching, peer support and local champions to give psychological motivation and encouragement. We are beginning to have some excellent discussions and develop some exciting plans around this.
I suggest that within a generation, if we wanted to, we could render Type 2 Diabetes a rare diagnosis. We can do this through encouraging far more healthy lifestyles in our children and young people now, like running a mile a day and learning to eat food that doesn’t actually harm them! I believe we could significantly reduce the need for so many people to be taking medication for hypertension and diabetes now, prevent many strokes and heart attacks, by being violent towards these conditions with major changes in lifestyle, though diet and exercise, rather than the prescription of drugs, using coaching, peer support and local champions to give psychological motivation and encouragement. We are beginning to have some excellent discussions and develop some exciting plans around this. pull themselves back from the brink of a lifetime of medication and we should use all medication reviews as a chance to help people adopt lifestyles that might reverse the need for such drugs. In the process, we would also significantly reverse our number of cancer diagnoses – many of which are linked to our lifestyle choices. We simply can’t afford for our current and failing approach to continue. We need to be braver together! And this means the NHS must be willing to partner in new ways, not only with local people, but also with businesses like the major supermarkets to help reverse our current direction towards the abyss, in which there is no longer a healthcare system that serves the needs of everyone, no matter where they come from or how much they do or don’t earn.
pull themselves back from the brink of a lifetime of medication and we should use all medication reviews as a chance to help people adopt lifestyles that might reverse the need for such drugs. In the process, we would also significantly reverse our number of cancer diagnoses – many of which are linked to our lifestyle choices. We simply can’t afford for our current and failing approach to continue. We need to be braver together! And this means the NHS must be willing to partner in new ways, not only with local people, but also with businesses like the major supermarkets to help reverse our current direction towards the abyss, in which there is no longer a healthcare system that serves the needs of everyone, no matter where they come from or how much they do or don’t earn. We can absolutely do this!! It’s going to take some serious resolve and we’re going to have to withstand the fear and pressure of some pretty powerful lobbies, like the sugar, alcohol, tobacco and pharmaceutical giants, and perhaps even the government itself, but it is time for us to do the impossible. With love, hope and faith, we can do this! Yes we need to focus on schools and work places. Yes, we need to partner with organisations we’ve never worked with before. Yes, we need a far more effective media strategy and yes, we need to allow clinicians to work very differently. But we cannot do nothing. So let’s try something a whole lot more radical. That’s what we’re going for in Morecambe Bay – not just better care together, but better health together – you can watch and wait, and see if we sink or swim, or you can join us!
We can absolutely do this!! It’s going to take some serious resolve and we’re going to have to withstand the fear and pressure of some pretty powerful lobbies, like the sugar, alcohol, tobacco and pharmaceutical giants, and perhaps even the government itself, but it is time for us to do the impossible. With love, hope and faith, we can do this! Yes we need to focus on schools and work places. Yes, we need to partner with organisations we’ve never worked with before. Yes, we need a far more effective media strategy and yes, we need to allow clinicians to work very differently. But we cannot do nothing. So let’s try something a whole lot more radical. That’s what we’re going for in Morecambe Bay – not just better care together, but better health together – you can watch and wait, and see if we sink or swim, or you can join us! have huge health inequalities. There are major issues with housing, economic policies that are not working for huge swathes of our population, with more people having to use food banks, struggling with fuel poverty, living in damp houses and unable to make ends meet. Yes, our kids are spending more time on screens and less time in activity. Yes, the sugar lobby, alcohol lobby and advertising giants have far too much power. Supermarkets are designed deliberately so that we buy things that are bad for us. And sometimes, we just make poor choices (if you can call them choices, which for some people, they aren’t always) – we do not all live as healthily as we could – we eat the wrong stuff, work highly stressful jobs, and exercise less than we are recommended to. Mental health issues are on the rise, especially for teenagers, due to crazy targets and league tables, with all the pressures they face. We are less happy and more separated than we ever used to be, despite the rise in social media…..(or maybe because of it……)…..Man, I can paint a negative picture – it’s like storm clouds and darkness everywhere……..
have huge health inequalities. There are major issues with housing, economic policies that are not working for huge swathes of our population, with more people having to use food banks, struggling with fuel poverty, living in damp houses and unable to make ends meet. Yes, our kids are spending more time on screens and less time in activity. Yes, the sugar lobby, alcohol lobby and advertising giants have far too much power. Supermarkets are designed deliberately so that we buy things that are bad for us. And sometimes, we just make poor choices (if you can call them choices, which for some people, they aren’t always) – we do not all live as healthily as we could – we eat the wrong stuff, work highly stressful jobs, and exercise less than we are recommended to. Mental health issues are on the rise, especially for teenagers, due to crazy targets and league tables, with all the pressures they face. We are less happy and more separated than we ever used to be, despite the rise in social media…..(or maybe because of it……)…..Man, I can paint a negative picture – it’s like storm clouds and darkness everywhere…….. But what if it wasn’t that way? What if we got a bit angry about it, but instead of finding someone to blame and pointing the finger; instead of getting all tribal and throwing stones at others, we chose to use our energies creatively to find solutions, to work together and make positive changes?! Let’s put away our pointing fingers and our ranting tongues and let’s work together for a better future for everyone! Doesn’t that sound good?! It’s what we’re trying here in Morecambe Bay, and I’m hoping it spreads like wild fire so that we can become a place where health abounds and beauty surrounds (that’s the motto of this place!). That doesn’t mean we stop speaking truth to power, but we also let our actions (and maybe our votes) speak louder than ever before.
But what if it wasn’t that way? What if we got a bit angry about it, but instead of finding someone to blame and pointing the finger; instead of getting all tribal and throwing stones at others, we chose to use our energies creatively to find solutions, to work together and make positive changes?! Let’s put away our pointing fingers and our ranting tongues and let’s work together for a better future for everyone! Doesn’t that sound good?! It’s what we’re trying here in Morecambe Bay, and I’m hoping it spreads like wild fire so that we can become a place where health abounds and beauty surrounds (that’s the motto of this place!). That doesn’t mean we stop speaking truth to power, but we also let our actions (and maybe our votes) speak louder than ever before. We’re talking together, taking time to dream about what it would be like if we were the healthiest area in the UK. We’re training up many people to host conversations, so that we break down walls and learn to collaborate for the sake of everyone. We’re not just dreaming about physical health, but mental, social and systemic health as well. We’re encouraging those who want to rise up and take some leadership, to be pioneers in the stuff they are passionate about. Even in my little town, we now have a mental health cafe that is literally saving people’s lives, because a lady called Jane wanted to make a difference. We have a cafe for all the people who have circulation problems because one of our nurses wanted to break people’s isolation and improve their healing rates at the same time.
We’re talking together, taking time to dream about what it would be like if we were the healthiest area in the UK. We’re training up many people to host conversations, so that we break down walls and learn to collaborate for the sake of everyone. We’re not just dreaming about physical health, but mental, social and systemic health as well. We’re encouraging those who want to rise up and take some leadership, to be pioneers in the stuff they are passionate about. Even in my little town, we now have a mental health cafe that is literally saving people’s lives, because a lady called Jane wanted to make a difference. We have a cafe for all the people who have circulation problems because one of our nurses wanted to break people’s isolation and improve their healing rates at the same time.  We’ve got a carers cafe, a dementia cafe and will soon have a breathing cafe for those who have severe COPD, sharing ideas and diminishing anxiety. We’ve got exercise classes to help with pain, a community choir, dog poo wardens to help us take more pride when we walk down the street and food banks to help those who can no longer afford to eat.
We’ve got a carers cafe, a dementia cafe and will soon have a breathing cafe for those who have severe COPD, sharing ideas and diminishing anxiety. We’ve got exercise classes to help with pain, a community choir, dog poo wardens to help us take more pride when we walk down the street and food banks to help those who can no longer afford to eat. We’re changing the way consultations happen in the NHS to enable people to make more informed and better choices about their own health and conditions, so they feel empowered to make changes that work for them rather than beaten up when they go for an appointment! We’re launching the Morecambe Bay Poverty Truth challenge, learning from those who are lived
We’re changing the way consultations happen in the NHS to enable people to make more informed and better choices about their own health and conditions, so they feel empowered to make changes that work for them rather than beaten up when they go for an appointment! We’re launching the Morecambe Bay Poverty Truth challenge, learning from those who are lived  experts in poverty to help us work together and care better for those most struggling in our society. We’re having difficult conversations about death to help people be prepared for every eventuality.
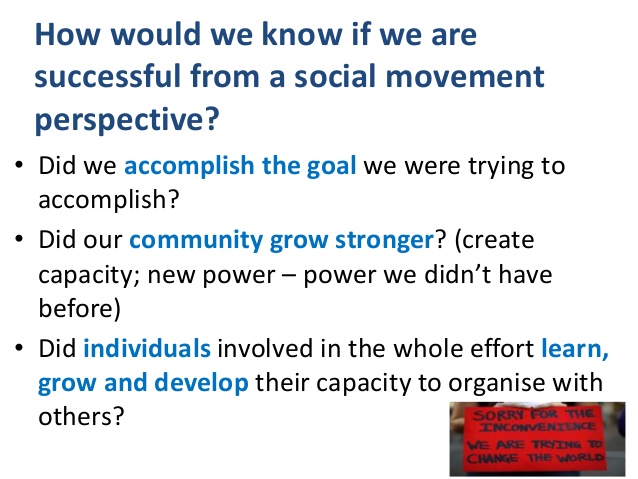
experts in poverty to help us work together and care better for those most struggling in our society. We’re having difficult conversations about death to help people be prepared for every eventuality. will be awakened? What other partnerships, collaborations and relationships might be formed? Being all tribal and accusatory of others saps our energy and stops us being creative. Mud slinging and blame will achieve little. We have to work from where we are. We have to build bridges and work together. We have to build a future of positive peace and that means binary thinking is over! The future doesn’t have to be full of doom and gloom. It is alive with hope! What resources might we find? What talents might we discover? What might we see develop over the next 12 months/years/decades as we look for solutions together for a better future for everybody? Don’t you feel just a little bit excited?
will be awakened? What other partnerships, collaborations and relationships might be formed? Being all tribal and accusatory of others saps our energy and stops us being creative. Mud slinging and blame will achieve little. We have to work from where we are. We have to build bridges and work together. We have to build a future of positive peace and that means binary thinking is over! The future doesn’t have to be full of doom and gloom. It is alive with hope! What resources might we find? What talents might we discover? What might we see develop over the next 12 months/years/decades as we look for solutions together for a better future for everybody? Don’t you feel just a little bit excited?