Who should take responsibility for you health? Sounds like a straightforward question, doesn’t it? But I get so frustrated when complex issues get squashed into simplified, silo-thinking, ready for twitter or media sound bites, or the under-girding of political ideologies.
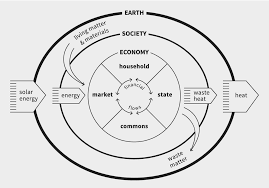
So….just as the economy is not just made up of the interplay between business and the household, but is in fact far more rich and complex, so too the interplay of responsibility for our own health.
Kate Raworth, really helpfully uses the following diagram to help us rethink the components of the economy. I would like to suggest that we use it to think about health, also.
So…who is responsible for your health and wellbeing?
- Your Family/Household
- Society/The Commons
- The Market
- The State
- You
In some ways, I feel like all of these are obvious, in their own way, but I will just unpack each one a little bit more.
Your Family/Household
We all have needs. We need to know we are provided for (water, food, clothes etc), safe, loved, welcome, encouraged, disciplined and given place to dream and live those dream out. It is the role of our families or the household to which we belong to ensure those things happen as we grow. So much of our ill-health, our brokenness and our long term physical and psychological pain is because these basic needs were never met and left us without a sense of wholeness. The lack of met need, has a huge impact on the development of our personality and character. When we speak of ‘personality disorders’, each type has it’s roots in early life when needs were unmet and therefore parts of the personality remained undeveloped. Let’s face it – no family is perfect! And so, I would argue, that all of us have ‘disordered personalities’, and until we confront the shadow parts of ourselves that are trying to overcome this sense of loss or inadequacy, we continue to project an ego version of ourselves to those around us. We do so to cover over this pain, but facing it head on and allowing ourselves to fess up to our deepest needs, would actually lead to us being a great deal more healthy.
When I work with head teachers and ask them what the biggest need they have in their school, the answer is almost always ‘parenting classes’. However, there are very few providers of this available (due to cuts at a county council level) and the classes available are often very ‘middle class’ in their approach. We need to completely rethink parenting classes in the context of the poverty-truth commission and think about less twee ways to really engage with communities about how we raise happy and healthy kids. The truth that Adverse Childhood Experiences are our greatest public health crisis is not going away. Grasping this nettle is going to be painful but really necessary if we are to breathe health and wellbeing into our society.
Society/The Commons
 Just as we get our needs met by those in our immediate household, the same is true of society. The way we treat children, the things we expose them to, the way we love them and educate them has a massive impact on their current future health and wellbeing. It’s becoming clear that social media is causing significant harm to our mental health as a nation, particularly our young people, and yet we don’t know how to curb our enthusiasm for all our technology…let alone the rise of the robots…
Just as we get our needs met by those in our immediate household, the same is true of society. The way we treat children, the things we expose them to, the way we love them and educate them has a massive impact on their current future health and wellbeing. It’s becoming clear that social media is causing significant harm to our mental health as a nation, particularly our young people, and yet we don’t know how to curb our enthusiasm for all our technology…let alone the rise of the robots…
The commons is fast disappearing, too easily privatized and made available to those who can afford it. How do we safeguard the commons and use it for the benefit of all? What would the Diggers say to us now? The breakdown of our communities, with increasing isolation and loneliness is having a detrimental effect on our wellbeing. What can we do to recover the spaces that belong to us all and help us rediscover the joy of connecting and being together?
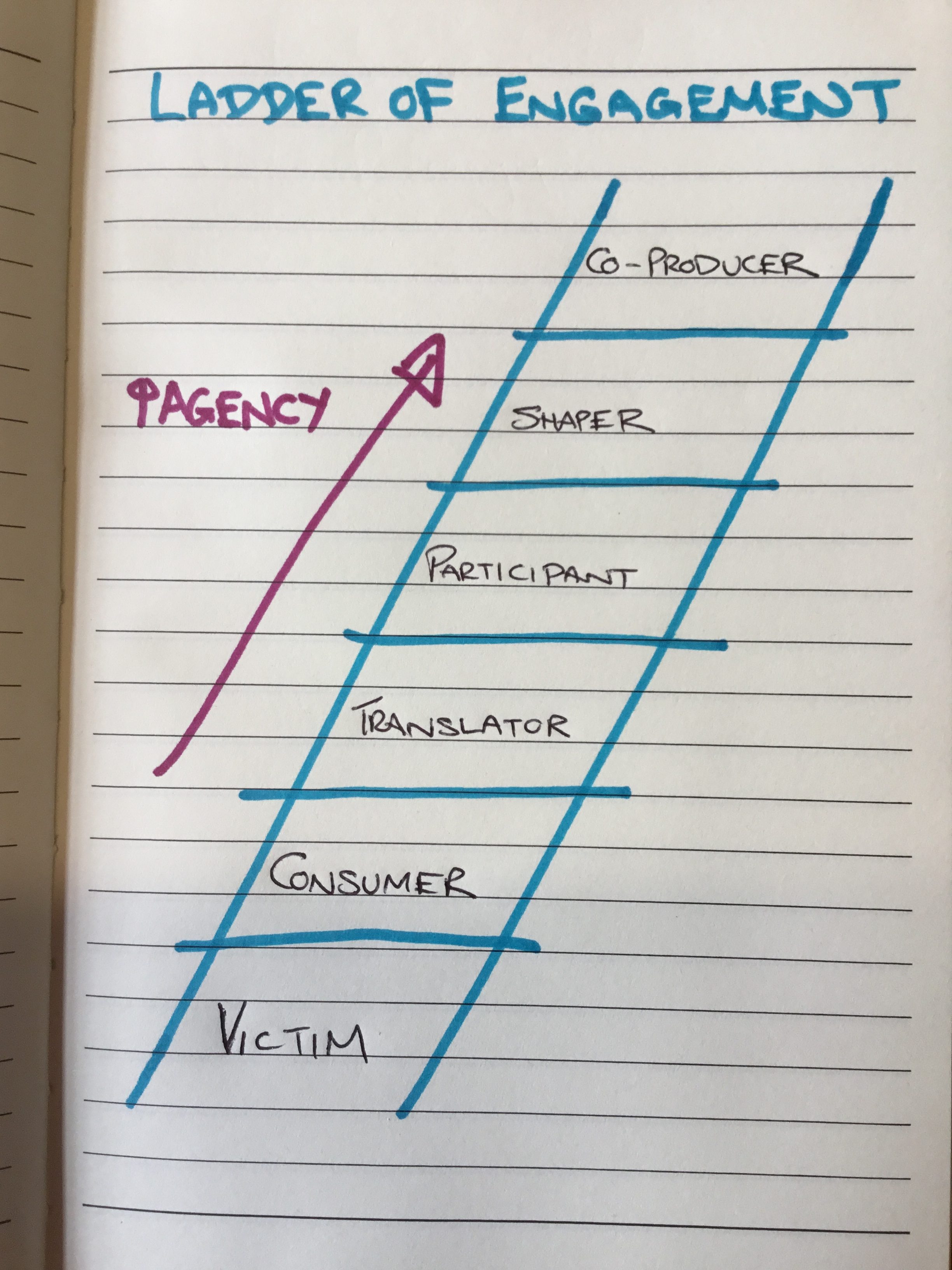
The commons is also about our corporate voice. It is only really vast people movements, speaking with one voice that can really cause governments to sit up, listen and take heed of the needs of the people. It is only together, that we will make enough noise to change the health and wellbeing of all of us for the better. How might we speak and act together in a way that will take corporate responsibility for all our health and wellbeing?
The Market
 Oh the benevolent hand of the market! If only…. But the Market plays an absolutely key (though currently over played) part in our economy and our health and wellbeing. We know for a fact that advertising is deliberately trying to misinform us so that we make irrational decisions. A key component is to make people feel worse about themselves so that they buy things they simply do not need. Supermarkets are being challenged for the ways they deliberately place products and arrange their stores to cause people to buy more unhealthy things and food chains are constantly trying to ‘up-sell’ their unhealthy products and downgrade our health in the process. They evangelize the masses with the idea that we are all free to make our own choices, but if this were so, they would not spend the billions of pounds involved in socially engineering our choices, so that we ‘freely’ choose that which harms us! Oh for a market that might redefine it’s moral code! The market could do SO much good, but unharnessed and left without true accountability or consequences, it serves to damage our health – something it is truly responsible for.
Oh the benevolent hand of the market! If only…. But the Market plays an absolutely key (though currently over played) part in our economy and our health and wellbeing. We know for a fact that advertising is deliberately trying to misinform us so that we make irrational decisions. A key component is to make people feel worse about themselves so that they buy things they simply do not need. Supermarkets are being challenged for the ways they deliberately place products and arrange their stores to cause people to buy more unhealthy things and food chains are constantly trying to ‘up-sell’ their unhealthy products and downgrade our health in the process. They evangelize the masses with the idea that we are all free to make our own choices, but if this were so, they would not spend the billions of pounds involved in socially engineering our choices, so that we ‘freely’ choose that which harms us! Oh for a market that might redefine it’s moral code! The market could do SO much good, but unharnessed and left without true accountability or consequences, it serves to damage our health – something it is truly responsible for.
The State
 The state has a vital role and responsibility in caring for all of our health and when it washes it’s hands of that responsibility or tries to pass it over, we see a massive rise in health inequalities and overall worse-health for all. The NHS in the UK is one of the great triumphs of the state. Providing brilliant healthcare for those who need it whenever they are unwell is truly amazing. Imagine not being able to afford this because it depended on keeping up with insurance bills. It is not uncommon for us to see people in General Practice, who literally cannot afford to feed their families any more and are having to make some incredibly difficult choices (made far worse by long school holidays). Easy to point the finger and start creating a narrative about how it’s “all their fault”, but far harder to hear the truth of what it is really like to be a lived-expert in poverty and the trap it creates and harder still to look to alternative solutions, rather than believe the austerity narrative. There is clear evidence that the more unequal a society becomes, the worse the health outcomes – both physical and mental. When the market is allowed to behave exactly as it wants, we also see the health of people suffer. It is only through the right kind of government that the market can be tamed. It is only with the right kind of legislation that the economy can be skewed towards redistribution and regeneration of the resources needed – this would need to include a radically feminist approach that works on behalf of women, in particular, for equal opportunity, pay and recognition of just how much the ‘household economy’ contributes to the overall wellbeing of the nation. It is only the right kind of leadership that will tackle the inequalities we see and refuse to be wined and dined into maintaining the status quo. It is only brave leadership that will take the ecological issues, like plastic in the oceans, massive over antibiotic use in animals, and ongoing air and river pollution that will give us a healthy planet and human population in the future.
The state has a vital role and responsibility in caring for all of our health and when it washes it’s hands of that responsibility or tries to pass it over, we see a massive rise in health inequalities and overall worse-health for all. The NHS in the UK is one of the great triumphs of the state. Providing brilliant healthcare for those who need it whenever they are unwell is truly amazing. Imagine not being able to afford this because it depended on keeping up with insurance bills. It is not uncommon for us to see people in General Practice, who literally cannot afford to feed their families any more and are having to make some incredibly difficult choices (made far worse by long school holidays). Easy to point the finger and start creating a narrative about how it’s “all their fault”, but far harder to hear the truth of what it is really like to be a lived-expert in poverty and the trap it creates and harder still to look to alternative solutions, rather than believe the austerity narrative. There is clear evidence that the more unequal a society becomes, the worse the health outcomes – both physical and mental. When the market is allowed to behave exactly as it wants, we also see the health of people suffer. It is only through the right kind of government that the market can be tamed. It is only with the right kind of legislation that the economy can be skewed towards redistribution and regeneration of the resources needed – this would need to include a radically feminist approach that works on behalf of women, in particular, for equal opportunity, pay and recognition of just how much the ‘household economy’ contributes to the overall wellbeing of the nation. It is only the right kind of leadership that will tackle the inequalities we see and refuse to be wined and dined into maintaining the status quo. It is only brave leadership that will take the ecological issues, like plastic in the oceans, massive over antibiotic use in animals, and ongoing air and river pollution that will give us a healthy planet and human population in the future.
You
 And where possible, and for some given various health issues, this is more possible for some than others – we do not all have an equal starting place or a level playing field – where we can – we do have a responsibility to ourselves and to the wider society to care for our own health and wellbeing, so that when the health and social services are needed, they are available for all. It also means using the health and social care services in a way that creates sustainability, being grateful for them and ensuring they and the people who work in them are not abused.
And where possible, and for some given various health issues, this is more possible for some than others – we do not all have an equal starting place or a level playing field – where we can – we do have a responsibility to ourselves and to the wider society to care for our own health and wellbeing, so that when the health and social services are needed, they are available for all. It also means using the health and social care services in a way that creates sustainability, being grateful for them and ensuring they and the people who work in them are not abused.
It’s complex, but it’s vital that too much emphasis is not put on any one area. We must not play the blame game, especially not towards individuals when we haven’t taken the time to hear their story, nor understood the wider context of the role of the other vital players on the field. Each aspect of the economy plays a massive role in the health and wellbeing of the nation, and it is high time that each plays it’s relevant part to its fullest ability.