On Friday night, watching comic relief, I got quite excited as the total neared £50 million – I turned to my lovely wife and said – ha – there now, we can plug the gap in our local health economy for next year! (Obviously the money is desperately needed in many situations across the UK and Africa, so I wasn’t being flippant), but – that’s the target we’ve been set by the government in Morecambe Bay – save £50 million pounds – one tenth of our budget in 1 year!! Sure thing! The public just love to hear about cuts! Comic relief – you have to laugh, or you’d cry……..but the situation isn’t really very funny and yet, if we don’t head into the fray with some joy and hope in our hearts, we will become wearied very quickly.
 Let me frame this problem by stating something we must then put to one side. Professor Don Berwick, health advisor to Barack Obama, and president of the IHI (Institute for Health Innovation at Harvard – a clever man by all accounts) recently stated very clearly to the Department of Health that it is quite simply not possibly to continue having a National Health Service run on only 8% of GDP (the lowest spend on healthcare of almost any OECD nation). We must also put to one side the recent publication by the King’s Fund, the independent think tank, that states quite clearly that the government are not investing anywhere near what they promised they would in the NHS. It also demonstrates that the NHS is not a bottomless pit, as some of the media would have us believe. Read it in more depth here:
Let me frame this problem by stating something we must then put to one side. Professor Don Berwick, health advisor to Barack Obama, and president of the IHI (Institute for Health Innovation at Harvard – a clever man by all accounts) recently stated very clearly to the Department of Health that it is quite simply not possibly to continue having a National Health Service run on only 8% of GDP (the lowest spend on healthcare of almost any OECD nation). We must also put to one side the recent publication by the King’s Fund, the independent think tank, that states quite clearly that the government are not investing anywhere near what they promised they would in the NHS. It also demonstrates that the NHS is not a bottomless pit, as some of the media would have us believe. Read it in more depth here:
(https://www.kingsfund.org.uk/topics/productivity-and-finance/nhs-myth-busters)
We know we need more funding. We know there is much negativity in the press about the crisis we are facing, we know about the recruitment issues and we know about the low morale of staff and high strain on the service.
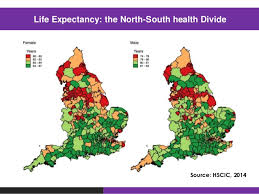
Having put all of that to one side and accepting that the NHS remains a political football, currently being given a good kicking, we do need to have a sensible conversation. Whether we like it or not, as we look into the future, it is unsustainable for the health and social care system to have to allocate 1/5th of its budget as a direct result of our lifestyles, 1/10th of its budget on diabetes (the vast majority relating to type II, which is hugely preventable and reversible) or to double pay for beds in nursing homes and hospitals  because of unnecessary admissions. So…..what are we to do? Simon Stevens, the head of the NHS will, this week give a major speech on the direction the health service and the progress of the Sustainability and Transformation Plans (STPs), of which there are 44 across England – they have little chance of success if we do not believe that we are all in this together.
because of unnecessary admissions. So…..what are we to do? Simon Stevens, the head of the NHS will, this week give a major speech on the direction the health service and the progress of the Sustainability and Transformation Plans (STPs), of which there are 44 across England – they have little chance of success if we do not believe that we are all in this together.
It truly involves all of us! We, the people, together must face this problem head on. We do not have to turn on each other in a time of crisis, we can turn to each other and use our collective wisdom and gifts to find a way through. This does not have to mean doom and gloom. It could mean better community cohesion, a more positive way of working together across the system, organisations working collaboratively in a way that makes more sense for those who need help and all of us taking a bit more responsibility for our own health and wellbeing. We must learn to rebuild the very fabric of society, based on love and trust, de-professionalise the public and civic space (as per Cormac Russell) and reconnect as human beings who care for each other and want to have systems that serve our needs. This will be made possible through multiple, small and large conversations in which we take time to ask some really deep and important questions, holding the space through the process of frustration as we wrestle together for solutions that we can all work with.We don’t leave our brains and expertise at the door, but nor do we behave in archaic hierarchical ways or hide behind our name badges and lanyards. Here in Morecambe Bay we have started this very process, using a set of values from ‘the art of hosting and harvesting conversations that matter’ – here is a link to one of our conversations in Morecambe:
http://aohhealthandwellbeingmorecombe.weebly.com
Over the next two years, our team will be working with communities right around this Bay to ask and explore some important questions, such as these:
- How do we begin well? Put another way – How do we enable our children to have the very best start in life? (This may include areas like breast feeding, bonding, parenting, healthy food, exercise and the massive public health issue that is child abuse – or adverse childhood experiences, or maybe issues like indoor vs outdoor learning, music, arts, sports, targets, sex, screen time, social media etc) – what are we going to do about this as a society?
- How do we live well? How do we face some of the issues we are now having to tackle? How do we square up to some of the nonsensical adverts, learn to laugh at them, rather than be sucked in by them and change the message?! How do we reconnect, heal our divides and learn to live well alongside each other? How do we heal our past traumas that have such a huge impact on our health and wellbeing now? How might we build the kind of economy that cares about people and the planet? How might we live in an altogether more healthy way? How do we become less dependent on a medical model to fix our problems and take a more holistic view of what it means to be well?
- How do we work well? How do we create work that cares for the future and sustainability of the planet? How do we work in ways that are beneficial to our health and by doing so actually help us to be more effective and efficient? How do we create a culture of kindness and compassion in our workplaces?
- How do we age well? How do face retirement, without it becoming only a selection of cruises and alcohol (biggest problem drinking now in women over 60)? How do we connect three generations back to each other and enjoy life more fully together? How do we live well with increasing frailty and health issues? How do we understand the conditions we live with and learn how to manage them ourselves (self-care) as effectively as possible? How do we create the kind of social care that is compassionate, caring and serves to create community?
- How do we die with dignity? We must ask ourselves some difficult questions here. Why do we admit so many people to hospital from nursing and residential homes, when there is little evidence that they get better any faster and then end up blocking the beds? Why are we not more radically reallocating resources out into the community to care for people in these settings and in their own homes? Why are we so afraid of our own mortality and allowing people to die well in environments that are familiar to them, surrounded, where possible, by people who know them and love them? How can we face our own deaths well and plan for them in a way that makes the end of our lives better for us and those around us?
If we take each of those questions in turn (as we plan to do) and really talk together about how we make society and therefore our health and wellbeing better for everyone, rather than leaving it to others to make those decisions from on high for us, then I think we will achieve more than we could ever imagine possible. It is in discovering one another, in encountering the other that we can be transformed and find new ways forward together.
A people movement or social movement such as this will invigorate and create space for those within the systems not only to reconnect with our own humanity but enable us also to have braver conversations about how we can share our resources more effectively, work together more creatively and reimagine how we can provide the kind of health and social care that makes sense for the needs of the people we serve. We might not save £50 million, but we can’t continue with things as they are and if we talk and work together, we could make a really difference.