This week, the Kingsfund, one of the most respected think-tanks on health and social care in the UK declared that the current NHS staffing levels are becoming a ‘national emergency’.
The latest figures have been published by the regulator, NHS Improvement, for the April to June period.
They showed:
■ 11.8% of nurse posts were not filled – a shortage of nearly 42,000
■ 9.3% of doctor posts were vacant – a shortage of 11,500
■ Overall, 9.2% of all posts were not filled – a shortage of nearly 108,000
NHS vacancies a ‘national emergency’
This is having a profound impact on staff who are working in the NHS now, with low morale, high stress levels, increasing mental health problems and people leaving the profession (either to go over seas, where pay and work-life balance is considerably better) or retire early.
Increasing the number of doctors, nurses and midwives (all with considerable debt, mind you!), by 25% over the next 5 years is welcome, but it doesn’t solve the problem now, and it is unlikely to be enough, even then!
But, let’s take a solutions focussed approach. What can we do now? I think there are a few things we need to consider:
- I can understand how frustrating it is for the public to find that waits are longer to receive much needed care. When we’re anxious or worried about our own heath or that of a loved one, we are understandably at a position of higher stress. However, this staffing crisis is not of the making of the nurses, doctors and other health professionals who work long hours every day to provide the best health care they can. So, it’s really important that as a country, we treat our NHS staff with kindness, gratitude and respect. The current abuse of NHS staff is making the job even harder and really making people not want to come to work. And that means we also need to make complaints in a way that is perhaps a bit more compassionate or understanding towards people who are working under high stress situations. It is important that we learn from mistakes, but complaints have a huge impact on staff and can hugely affect their confidence, even when they are dealt with in a very compassionate way by those in leadership.
- We need to ensure that we use our appointments appropriately. Yes – sometimes, we have to wait a while to see our GP, but if we get better in the mean time, we really don’t need to be keeping the appointment! And missing appointments costs us all so much time and energy and makes those waiting lists ever longer. If we value our health system, we need to either keep appointments, or take responsibility to cancel them.
- We need to take an urgent look at the working day of our NHS staff and work out how we build more health and wellbeing breaks into their days. We need staff to have space to connect, keep learning, be active, be mindful and take appropriate breaks. This means senior leadership teams getting the culture right, when the pressure is on and the stakes are high.
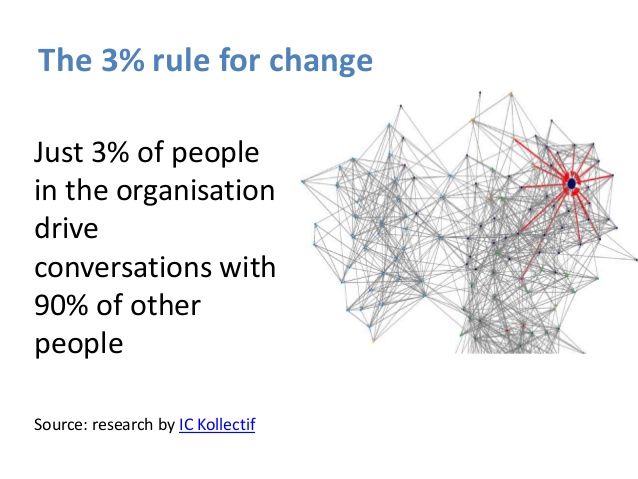
- We need to get smarter with digital and enable patients to make better and more informed choices about their own care and treatment, with better access to their notes. In this way, we waste less time and empower people to become greater experts in the conditions with which they live everyday. There are great examples of where this is happening already. It isn’t rocket science and can be rolled out quite easily. It’s good to see some announcements about this from the new health secretary Matt Hancock MP, but we need to make sure the deals and the products are the right ones. It’s also vital, when it comes to digital solutions that Matt Hancock listens to his colleague and chair of the health select committee, Dr Sarah Wollaston MP, in being careful what he promotes and prioritises.
- We need to be thinking NOW about the kind of workforce we are going to need in the next 2-3, and 5-10 years and we need to get the training and expectations right now! There is no point designing our future workforce based on our current needs. Rather, we need expert predictive analysis of the kind of future workforce we will need, in line with the ‘10 year plan’ and begin to grow that workforce now. If it’s healthcoaches we need to work alongside GP practices, then let’s get them ready, if it’s community focussed nursing teams, then let’s adjust the training programmes. This kind is vital and must influence what happens next.
- We need to stop putting pressure on NHS staff to deliver that which is currently undeliverable without causing significant stress to an already overstretched workforce. By this I mean centrally driven schemes, such as the intended roll out of GPs working 8-8, 7 days a week. Maybe it’s an aspiration for the future if we can sufficiently reimagine the workforce, but it’s not a priority now and isn’t the answer to the problems we’re facing.
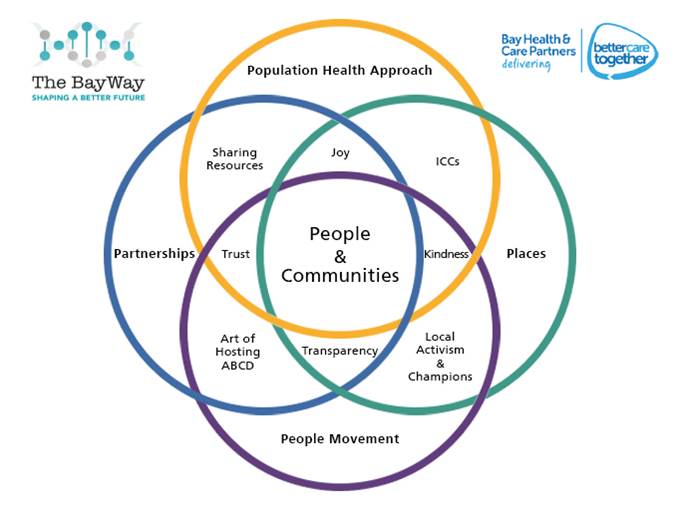
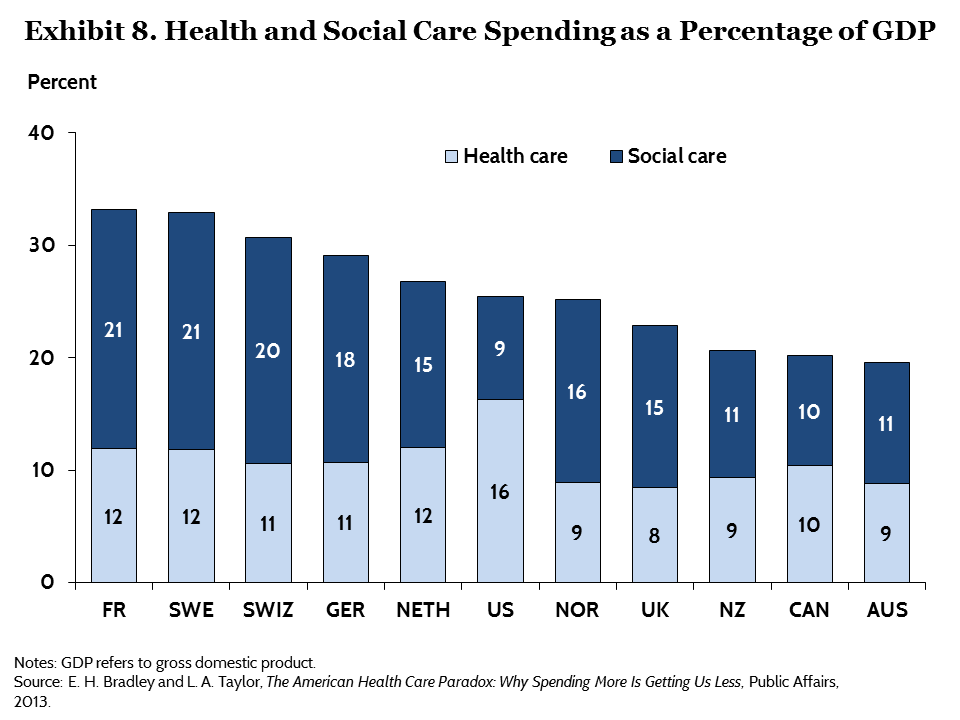
- We need to stop the cutting of social care in local governments, and ensure that central funding flows to where it needs to be, to ensure the allied support services are present in local communities to work alongside NHS colleagues in getting the right care in the right place at the right time. This is the single biggest cause of our long ED waits and our problems with delayed discharges from hospital. It isn’t rocket science. It’s the reality of cuts to our social care provision, which have been too deep and this needs to be reversed.
Personally, although it is an option, I feel uncomfortable about a ‘recruitment drive’ from overseas, as it is very de-stabilising to health care systems in more deprived parts of the world when we do that. I think there are some win-win initiative we could develop pretty quickly that could also form part of our international development strategy.
In summary, we need to treat our NHS staff with kindness, look after their wellbeing, use our services appropriately, use digital technology with wisdom and not for political gain, redesign and start building the workforce of the future now, stop undeliverable initiatives and ensure the right funding and provision of services through social care which means central government funding back into local government. It won’t solve everything, but it will go along way towards giving us a more sustainable future to the NHS.