I spoke at the NHS innovation agency north west yesterday about using video in engagement. Here is a 2 minute summary of some of what I shared!
I spoke at the NHS innovation agency north west yesterday about using video in engagement. Here is a 2 minute summary of some of what I shared!
Here are some excerpts from a speech I gave recently at Lancaster City Hall about how in a time of crisis, we can either turn on each other, or turn to each other (my friend Mike Love gave me that line!). When we turn to each other, unimagined possibilities become the fuel of hope for a better future for us all. I broke the 20 minute speech into just over 6 minutes – sorry if it’s a bit clunky, but I hope you get the gist!
Following on from my blog earlier this week, I want to be really clear in what I am saying!
My argument is this: if the correct investment was made, the formula wasn’t weighted against us and we therefore received the correct allocation of resource according to the task ahead of us, we would actually probably be in surplus and could really make a difference – we are already doing loads of great stuff, but asking us to make bricks with no straw is beyond the pale.…..as it is, what we’re being asked to do may affect the health and wellbeing of our population negatively because we are already at such a deficit, before we start….
This is not a political issue – this IS a Social Justice issue.
 Everybody knows about the Gender Pay Gap – it’s well publicised and very much in the public domain for discussion – and too right! – How is this even still an issue? It it is quite simply wrong that women should earn less than men, any time, any place, end of discussion.
Everybody knows about the Gender Pay Gap – it’s well publicised and very much in the public domain for discussion – and too right! – How is this even still an issue? It it is quite simply wrong that women should earn less than men, any time, any place, end of discussion.
Well the same applies to the North-South Health Gap. What I find particularly irksome about this issue, is that people tend to roll their eyes and say that it’s all playing politics. No! No it isn’t. This is not about politics. This is about Social Justice!
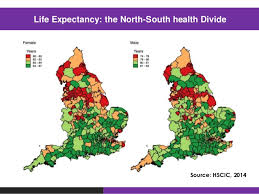 It has been well documented that for over 40 years, the health of the people of the North of England has been significantly worse than that of people in the South and our life expectancy is worse. It is a complex issue and is highly linked to deprivation and poor housing conditions in the urban areas. The gap was narrowed during the early part of this century, but the health reforms made to the NHS have seen massive cuts to public health and social care budgets, disproportionately affecting the North. To make matters worse, the funding formula that is used by the Department of Health to determine how and where money should be spent, deliberately favours the rich and the well and and that means that head for head of population, the North does considerably worse than the South in terms of how much resource is made available. This is even true of how many staff are given proportionally to the North compared to the South. This is just ludicrous and is simply not fair. How can it make any sense at all to spend more money in areas where the population is more healthy and people have a significantly better overall life expectancy already? Are we to believe that Southerners are more important than Northerners, just as the pay gap would imply that men are more important than women?
It has been well documented that for over 40 years, the health of the people of the North of England has been significantly worse than that of people in the South and our life expectancy is worse. It is a complex issue and is highly linked to deprivation and poor housing conditions in the urban areas. The gap was narrowed during the early part of this century, but the health reforms made to the NHS have seen massive cuts to public health and social care budgets, disproportionately affecting the North. To make matters worse, the funding formula that is used by the Department of Health to determine how and where money should be spent, deliberately favours the rich and the well and and that means that head for head of population, the North does considerably worse than the South in terms of how much resource is made available. This is even true of how many staff are given proportionally to the North compared to the South. This is just ludicrous and is simply not fair. How can it make any sense at all to spend more money in areas where the population is more healthy and people have a significantly better overall life expectancy already? Are we to believe that Southerners are more important than Northerners, just as the pay gap would imply that men are more important than women?
The savings being asked of the Northern STPs (Sustainability and Transformation Plans) at a time in which we are already struggling with the huge cuts previously mentioned, and starting from a significant deficit in terms of our health outcomes, is meaning that the health and wellbeing of the people of the North will suffer further. I am not suggesting that we can not work more efficiently and collaboratively within the public services, nor am I suggesting that the people of the North do not need to take greater responsibility for our own health (although it is well known, that when you are more deprived, you are less likely to have the mental wellbeing to make positive choices about your own health). What I am saying is this: whatever the budget allocations may be; let them be fair!
Yes, it is time for us to tackle the health problems across the North, and we will do so together as the people. Maybe we don’t have carte blanche any more and have to reassess what we think might be available in terms of health care provision. But what we would like is to be able to make this journey by starting on a basis of equality with the South. No more North-South divide. No more unfair funding calculations. No more political games. Social-Health Justice for all, now.
For further information, you can read:
https://academic.oup.com/jpubhealth/article/37/1/34/1556643/Grim-up-North-or-Northern-grit-Recessions-and-the
https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/inequalities-in-life-expectancy-kings-fund-aug15.pdf#page2
http://councilportal.cumbria.gov.uk/documents/s50047/STP%20April%20submission%20for%20Lancashire%20and%20South%20Cumbria.pdf?nobdr=2
So, I was interviewed on BBC News 24 on Monday evening (sorry for the poor visual quality), to talk about why it is that we are so inactive in the North West (worst in the country, apparently at 47% being inactive).
We have also pretty much the worst health outcomes, with high rates of obesity, heart disease and Type II Diabetes. Maybe we can muster our Northern Spirit and do something about this together? We may have the odds stacked against us with the weather (!), our work-life balance, long working hours and various other factors, but being active is so good for us and helps our health in so many ways – let’s cut the excuses eh? Maybe it’s time for a cultural shift?! Time for healthier workplaces.
 My morning surgery began today with a patient of mine, who works as Health Care Assistant (or Band 3) in our local acute hospital trust. As we find across the board in the NHS right now, there are pressures in her department with under-staffing and a very high and demanding work load. She started her day in tears, telling me about the sleepless nights, but even more so about the lack of support she is feeling in her work environment. She feels unable to understand why huge fees are paid to find locum consultants, when posts are not covered, but money cannot be found for the absence of staff at her level, when the numbers are down, leading to an increased pressure and low morale.
My morning surgery began today with a patient of mine, who works as Health Care Assistant (or Band 3) in our local acute hospital trust. As we find across the board in the NHS right now, there are pressures in her department with under-staffing and a very high and demanding work load. She started her day in tears, telling me about the sleepless nights, but even more so about the lack of support she is feeling in her work environment. She feels unable to understand why huge fees are paid to find locum consultants, when posts are not covered, but money cannot be found for the absence of staff at her level, when the numbers are down, leading to an increased pressure and low morale.
 Now, this is not a criticism of the acute trust we partner with every day, because I actually know all too well the situation here, how complex it can be and just how dedicated to caring for staff the leadership of the trust are. However, when we read in the press today about sickness absence for stress among paramedics, and if I were to detail more stories about the number of cases I am currently dealing with as a GP about stress in the workplace for ALL grades of staff in the NHS and social care setting, then we have to face up to the fact that we have a problem. Stress in the workplace and low morale in our teams is not a problem we can afford to ignore. It not only causes high sickness rates, which then increases the pressure on teams, with knock on financial implications to the system; it also causes significant compassion fatigue (i.e. staff are literally less able to care about or for their patients), because they are emotionally overwhelmed, under-resourced and therefore become more numb, disengaged and unkind and this is detrimental to patient care.
Now, this is not a criticism of the acute trust we partner with every day, because I actually know all too well the situation here, how complex it can be and just how dedicated to caring for staff the leadership of the trust are. However, when we read in the press today about sickness absence for stress among paramedics, and if I were to detail more stories about the number of cases I am currently dealing with as a GP about stress in the workplace for ALL grades of staff in the NHS and social care setting, then we have to face up to the fact that we have a problem. Stress in the workplace and low morale in our teams is not a problem we can afford to ignore. It not only causes high sickness rates, which then increases the pressure on teams, with knock on financial implications to the system; it also causes significant compassion fatigue (i.e. staff are literally less able to care about or for their patients), because they are emotionally overwhelmed, under-resourced and therefore become more numb, disengaged and unkind and this is detrimental to patient care.
The problem is actually really complex, but it is, in my opinion, primarily cultural, and particularly affects the lower pay-grades of staff, because they feel and are in fact less able, to influence change. If we do not develop a culture of kindness towards our own teams and have a sea-change within our working environments in terms of how we care for each other, we will only see the problems go from bad to worse. So, how do we create a culture of kindness, a culture of honour, a culture of wellbeing?
I would like to suggest six things (all beginning with H – the 6Hs), which are fairly simple, but make a massive difference to how teams function and therefore the morale within those teams:
 Humanity – First, we must recognise that hierarchy has the inbuilt tendency to de-humanise us. As we get higher in the pyramidal systems in which we work, we can easily lose our humility and compassion towards others as we have to cope with the greater demands from “above us” and if we’re not careful we can turn into slave drivers. Top down, controlling leadership is detrimental to good morale and stifles teams from working effectively. There is a famous, ancient parable (told in the New Testament) about an unmerciful manager, who owed a huge amount of money to his master/CEO. The CEO called him to account and threatened to fire him. However, he begged for mercy and the master cancelled his debt and gave him a fresh chance. However, this same manager then went and found all the people who owed something to him, and instead of paying forward the mercy he had received, treated his own debtors shamefully, despite their begging and pleading for mercy. When the CEO found out about this, the manager was duly fired. I wonder how often we tolerate ‘bullying’ by managers, because they ‘run a tight ship’, without calculating the cost of this style of management on our teams and the patients we serve? Changing culture is hard. Even if the CEO sets a good culture, any one of us can bring a negative influence in the area we work. We have to make a conscious choice to keep our kindness switched on. As we climb the ladder of responsibility, we must continue to act with humanity. We must also remember that it works the other way round – we can start dehumanising those in leadership positions ‘above us’, or those who work in different teams. We make terribly unfair assumptions about people all the time. A little bit of understanding, kindness and compassion goes a HUGE way in treating each other with kindness instead of suspicion.
Humanity – First, we must recognise that hierarchy has the inbuilt tendency to de-humanise us. As we get higher in the pyramidal systems in which we work, we can easily lose our humility and compassion towards others as we have to cope with the greater demands from “above us” and if we’re not careful we can turn into slave drivers. Top down, controlling leadership is detrimental to good morale and stifles teams from working effectively. There is a famous, ancient parable (told in the New Testament) about an unmerciful manager, who owed a huge amount of money to his master/CEO. The CEO called him to account and threatened to fire him. However, he begged for mercy and the master cancelled his debt and gave him a fresh chance. However, this same manager then went and found all the people who owed something to him, and instead of paying forward the mercy he had received, treated his own debtors shamefully, despite their begging and pleading for mercy. When the CEO found out about this, the manager was duly fired. I wonder how often we tolerate ‘bullying’ by managers, because they ‘run a tight ship’, without calculating the cost of this style of management on our teams and the patients we serve? Changing culture is hard. Even if the CEO sets a good culture, any one of us can bring a negative influence in the area we work. We have to make a conscious choice to keep our kindness switched on. As we climb the ladder of responsibility, we must continue to act with humanity. We must also remember that it works the other way round – we can start dehumanising those in leadership positions ‘above us’, or those who work in different teams. We make terribly unfair assumptions about people all the time. A little bit of understanding, kindness and compassion goes a HUGE way in treating each other with kindness instead of suspicion. Humility – For those in leadership, there can be a tendency to forget that when we were in in ‘lower’ positions, we often felt the same low morale and pressure from those ‘above us’. Leadership requires that we keep our love and compassion switched on towards those who we now lead. This means we must really learn to listen, and that means having the humility to recognise where we have been getting it wrong. If we are not prepared to change, then we are not really listening. It takes courage to create a culture in which we can receiving a challenge from those in our team and be able to make a change and not just use our position to squash the person who dared to speak out. It takes even more guts to admit where we have been wrong, say sorry and move forward differently.
Humility – For those in leadership, there can be a tendency to forget that when we were in in ‘lower’ positions, we often felt the same low morale and pressure from those ‘above us’. Leadership requires that we keep our love and compassion switched on towards those who we now lead. This means we must really learn to listen, and that means having the humility to recognise where we have been getting it wrong. If we are not prepared to change, then we are not really listening. It takes courage to create a culture in which we can receiving a challenge from those in our team and be able to make a change and not just use our position to squash the person who dared to speak out. It takes even more guts to admit where we have been wrong, say sorry and move forward differently. Help – one of the very worst things that can happen in any team dynamic is when we hear the words ‘it’s not my job’. I hear it so often and it makes me sad! We must never think we are above any task – whether that is cleaning up a mess, wiping a patient’s bum or picking up some litter. We must simply help each other out. But we also need the humility to admit when we are struggling and actually ask for help. We encounter terrible and unspeakable trauma at times, or may simply be going through tough personal circumstances. Sometimes, we need the humility to recognise where we are not coping, where we are struggling, when we’re not functioning and ask for help. And when we ask for help we need to have the confidence that we will encounter the humanity of those around us to help us at our time of need.
Help – one of the very worst things that can happen in any team dynamic is when we hear the words ‘it’s not my job’. I hear it so often and it makes me sad! We must never think we are above any task – whether that is cleaning up a mess, wiping a patient’s bum or picking up some litter. We must simply help each other out. But we also need the humility to admit when we are struggling and actually ask for help. We encounter terrible and unspeakable trauma at times, or may simply be going through tough personal circumstances. Sometimes, we need the humility to recognise where we are not coping, where we are struggling, when we’re not functioning and ask for help. And when we ask for help we need to have the confidence that we will encounter the humanity of those around us to help us at our time of need. Honour – Sometimes a situation may not be able to change, but in these situations the very worst thing leaders can do is close ranks, shut communication down and raise the levels of demand. No, vulnerability, openness and honesty, sharing the reality of the situation and communicating clearly why things cannot change currently at least allows the team to pull together and face the situation as one. However, there must be a very clear challenge here – Yanis Varoufakis puts it so well in his book “And The Weak Suffer What they Must” – we have to remember just how crippling powerlessness can be. Like my patient this morning, she has no access to the ‘powers’ or to the ‘purse strings’. She cannot up and leave, she simply can’t afford to, and so she works under huge pressure for very little pay, powerless to enact change, other than to put in place her own boundaries. A cultural shift towards a culture of kindness is to ensure that those with the least ‘honour’ are treated the most honourably. Leadership is about being able to take the hit, not self-protectionism at the cost of ones team. It is absolutely amazing just how far the words ‘Thank You’ can go, to keeping this sense of honour alive.
Honour – Sometimes a situation may not be able to change, but in these situations the very worst thing leaders can do is close ranks, shut communication down and raise the levels of demand. No, vulnerability, openness and honesty, sharing the reality of the situation and communicating clearly why things cannot change currently at least allows the team to pull together and face the situation as one. However, there must be a very clear challenge here – Yanis Varoufakis puts it so well in his book “And The Weak Suffer What they Must” – we have to remember just how crippling powerlessness can be. Like my patient this morning, she has no access to the ‘powers’ or to the ‘purse strings’. She cannot up and leave, she simply can’t afford to, and so she works under huge pressure for very little pay, powerless to enact change, other than to put in place her own boundaries. A cultural shift towards a culture of kindness is to ensure that those with the least ‘honour’ are treated the most honourably. Leadership is about being able to take the hit, not self-protectionism at the cost of ones team. It is absolutely amazing just how far the words ‘Thank You’ can go, to keeping this sense of honour alive. Health – (by health, I mean wellbeing in its widest sense) – we have to actually care for the people around us. We have developed a culture in the NHS and social care where we will do all we can to care for our patients/clients, but will break the backs of ourselves or our teams in the process, which is actually entirely self-defeating! It is impossible to care for others well, when you are feeling exhausted and broken! I have said it on this blog before and I will say it many times again: we have to develop a sense of the health and wellbeing of the people in our teams. We need time in the craziness and business of each day to stop the mad rushing, be still and take notice/be mindful/be heartful. We all need time to get up off our chairs and stretch and be more active – #runamile every day (it only takes 15 minutes). We need time to connect with each other (do we really take time to know the people we spend an inordinate amount of time with and alongside and check they are actually doing OK?), to eat well, stay hydrated and keep learning, so we don’t feel overwhelmed. Building these as an absolute priority into our daily work routines is vital, especially as pressures increase. The tendency is that when the going gets tough, our health gets significantly worse. We must learn to protect this in the midst of our business, or we will suffer the consequences in multiple ways.
Health – (by health, I mean wellbeing in its widest sense) – we have to actually care for the people around us. We have developed a culture in the NHS and social care where we will do all we can to care for our patients/clients, but will break the backs of ourselves or our teams in the process, which is actually entirely self-defeating! It is impossible to care for others well, when you are feeling exhausted and broken! I have said it on this blog before and I will say it many times again: we have to develop a sense of the health and wellbeing of the people in our teams. We need time in the craziness and business of each day to stop the mad rushing, be still and take notice/be mindful/be heartful. We all need time to get up off our chairs and stretch and be more active – #runamile every day (it only takes 15 minutes). We need time to connect with each other (do we really take time to know the people we spend an inordinate amount of time with and alongside and check they are actually doing OK?), to eat well, stay hydrated and keep learning, so we don’t feel overwhelmed. Building these as an absolute priority into our daily work routines is vital, especially as pressures increase. The tendency is that when the going gets tough, our health gets significantly worse. We must learn to protect this in the midst of our business, or we will suffer the consequences in multiple ways. Hope – there is an ancient proverb that says: “hope deferred makes the heart sick, but hope coming is a tree of life.” Hopelessness takes root when we feel that nothing can ever change and we feel powerless to influence anything. Hope is born when we develop ways of working in which teams can work together on solutions to the problems they are encountering, rather than being dictated to from on high in a unrelational way. Hope is about being able to sense that the future is alive with possibility. It is a life line when things are tough, when the tunnel is long and dark – just a little glimpse of light – and then faith builds that together we can get there.
Hope – there is an ancient proverb that says: “hope deferred makes the heart sick, but hope coming is a tree of life.” Hopelessness takes root when we feel that nothing can ever change and we feel powerless to influence anything. Hope is born when we develop ways of working in which teams can work together on solutions to the problems they are encountering, rather than being dictated to from on high in a unrelational way. Hope is about being able to sense that the future is alive with possibility. It is a life line when things are tough, when the tunnel is long and dark – just a little glimpse of light – and then faith builds that together we can get there.
Not difficult. Actually pretty straight forward. We don’t need unkindness or low morale in our work places. We don’t want to be suffering with compassion fatigue because we are physically and emotionally drained and running on empty. We really can create the kind of culture we want to see and experience in the NHS and social care – a culture of kindness – sounds nice doesn’t it?! All it takes is for us to remember humanity, humility, help, honour, health and hope.
 Every day in Morecambe Bay 2000 children aged 4-11 run a mile a day (how fantastic is that?!). Inspired initially by the story from Stirling, the word is spreading and we now have another 3000 children starting across Lancashire. Our early data shows that there has been a dramatic improvement in the children’s health, from a physical, mental and educational perspective. 15 minutes a day for a healthier, happier child who is able to sleep better and concentrate more in class – it’s an absolute no brainer. And what is more – if it’s good for the kids, then it’s good for us all. We will all be more physically healthy, more mentally well and be more productive in our work if we just take a break (especially in that post-lunch lull) and do some exercise! Who amongst can’t spare 15 minutes a day? And for those who can’t run, there are other alternatives. Some of our kids here are cycling or walking or even using hand bikes according to their physical ability, but everyone is taking part. Even on rainy days, they just get out there, or if it’s especially vile, they do some aerobics or zumba in the classroom.
Every day in Morecambe Bay 2000 children aged 4-11 run a mile a day (how fantastic is that?!). Inspired initially by the story from Stirling, the word is spreading and we now have another 3000 children starting across Lancashire. Our early data shows that there has been a dramatic improvement in the children’s health, from a physical, mental and educational perspective. 15 minutes a day for a healthier, happier child who is able to sleep better and concentrate more in class – it’s an absolute no brainer. And what is more – if it’s good for the kids, then it’s good for us all. We will all be more physically healthy, more mentally well and be more productive in our work if we just take a break (especially in that post-lunch lull) and do some exercise! Who amongst can’t spare 15 minutes a day? And for those who can’t run, there are other alternatives. Some of our kids here are cycling or walking or even using hand bikes according to their physical ability, but everyone is taking part. Even on rainy days, they just get out there, or if it’s especially vile, they do some aerobics or zumba in the classroom.
The challenge is this: if kids 4-11 can move a mile a day…..can’t we all? What if it became part of our culture, here in Morecambe Bay and further afield that everyone is given space in their educational or working day to run or move one mile each day? One mile – 15 minutes – easy!
 Today, Simon Stevens, head of the NHS, will highlight that we are now half way through the 5 year period he launched to help transform the NHS. Across the UK, there are now 44 STPs (these stand for Sustainability and Transformation Plans). In order for the NHS to be sustainable in the future, there needs to be some transformation – it’s simple really. There are plenty of conversations happening about how the system itself can work more efficiently and many new ways of working are being trialled and forged. However, we all also need to transform the way we are living, as our current lifestyles are making the NHS have to deal with pressures it simply can’t cope with anymore. Part of our work as an STP in Lancashire is to work with our population to encourage us all to be more healthy and well in our daily lives. It isn’t rocket science. Simple, small steps go a long way to making significant changes to our health. The 4-11 year olds have laid down the gauntlet – one mile a day – a simple first step that packs a real punch. The NHS and City Council will be following in their wake. One of our headteachers lost 3 stone in 6 months just by following their lead…….let’s get moving, let’s be healthier and let’s have an NHS that is therefore more sustainable for the future. The Morecambe Bay Mile a Day could easily become the UK Mile a Day. (Also see The Daily Mile Foundation).
Today, Simon Stevens, head of the NHS, will highlight that we are now half way through the 5 year period he launched to help transform the NHS. Across the UK, there are now 44 STPs (these stand for Sustainability and Transformation Plans). In order for the NHS to be sustainable in the future, there needs to be some transformation – it’s simple really. There are plenty of conversations happening about how the system itself can work more efficiently and many new ways of working are being trialled and forged. However, we all also need to transform the way we are living, as our current lifestyles are making the NHS have to deal with pressures it simply can’t cope with anymore. Part of our work as an STP in Lancashire is to work with our population to encourage us all to be more healthy and well in our daily lives. It isn’t rocket science. Simple, small steps go a long way to making significant changes to our health. The 4-11 year olds have laid down the gauntlet – one mile a day – a simple first step that packs a real punch. The NHS and City Council will be following in their wake. One of our headteachers lost 3 stone in 6 months just by following their lead…….let’s get moving, let’s be healthier and let’s have an NHS that is therefore more sustainable for the future. The Morecambe Bay Mile a Day could easily become the UK Mile a Day. (Also see The Daily Mile Foundation).
On Friday night, watching comic relief, I got quite excited as the total neared £50 million – I turned to my lovely wife and said – ha – there now, we can plug the gap in our local health economy for next year! (Obviously the money is desperately needed in many situations across the UK and Africa, so I wasn’t being flippant), but – that’s the target we’ve been set by the government in Morecambe Bay – save £50 million pounds – one tenth of our budget in 1 year!! Sure thing! The public just love to hear about cuts! Comic relief – you have to laugh, or you’d cry……..but the situation isn’t really very funny and yet, if we don’t head into the fray with some joy and hope in our hearts, we will become wearied very quickly.
 Let me frame this problem by stating something we must then put to one side. Professor Don Berwick, health advisor to Barack Obama, and president of the IHI (Institute for Health Innovation at Harvard – a clever man by all accounts) recently stated very clearly to the Department of Health that it is quite simply not possibly to continue having a National Health Service run on only 8% of GDP (the lowest spend on healthcare of almost any OECD nation). We must also put to one side the recent publication by the King’s Fund, the independent think tank, that states quite clearly that the government are not investing anywhere near what they promised they would in the NHS. It also demonstrates that the NHS is not a bottomless pit, as some of the media would have us believe. Read it in more depth here:
Let me frame this problem by stating something we must then put to one side. Professor Don Berwick, health advisor to Barack Obama, and president of the IHI (Institute for Health Innovation at Harvard – a clever man by all accounts) recently stated very clearly to the Department of Health that it is quite simply not possibly to continue having a National Health Service run on only 8% of GDP (the lowest spend on healthcare of almost any OECD nation). We must also put to one side the recent publication by the King’s Fund, the independent think tank, that states quite clearly that the government are not investing anywhere near what they promised they would in the NHS. It also demonstrates that the NHS is not a bottomless pit, as some of the media would have us believe. Read it in more depth here:
(https://www.kingsfund.org.uk/topics/productivity-and-finance/nhs-myth-busters)
We know we need more funding. We know there is much negativity in the press about the crisis we are facing, we know about the recruitment issues and we know about the low morale of staff and high strain on the service.
Having put all of that to one side and accepting that the NHS remains a political football, currently being given a good kicking, we do need to have a sensible conversation. Whether we like it or not, as we look into the future, it is unsustainable for the health and social care system to have to allocate 1/5th of its budget as a direct result of our lifestyles, 1/10th of its budget on diabetes (the vast majority relating to type II, which is hugely preventable and reversible) or to double pay for beds in nursing homes and hospitals  because of unnecessary admissions. So…..what are we to do? Simon Stevens, the head of the NHS will, this week give a major speech on the direction the health service and the progress of the Sustainability and Transformation Plans (STPs), of which there are 44 across England – they have little chance of success if we do not believe that we are all in this together.
because of unnecessary admissions. So…..what are we to do? Simon Stevens, the head of the NHS will, this week give a major speech on the direction the health service and the progress of the Sustainability and Transformation Plans (STPs), of which there are 44 across England – they have little chance of success if we do not believe that we are all in this together.
It truly involves all of us! We, the people, together must face this problem head on. We do not have to turn on each other in a time of crisis, we can turn to each other and use our collective wisdom and gifts to find a way through. This does not have to mean doom and gloom. It could mean better community cohesion, a more positive way of working together across the system, organisations working collaboratively in a way that makes more sense for those who need help and all of us taking a bit more responsibility for our own health and wellbeing. We must learn to rebuild the very fabric of society, based on love and trust, de-professionalise the public and civic space (as per Cormac Russell) and reconnect as human beings who care for each other and want to have systems that serve our needs. This will be made possible through multiple, small and large conversations in which we take time to ask some really deep and important questions, holding the space through the process of frustration as we wrestle together for solutions that we can all work with.We don’t leave our brains and expertise at the door, but nor do we behave in archaic hierarchical ways or hide behind our name badges and lanyards. Here in Morecambe Bay we have started this very process, using a set of values from ‘the art of hosting and harvesting conversations that matter’ – here is a link to one of our conversations in Morecambe:
http://aohhealthandwellbeingmorecombe.weebly.com
Over the next two years, our team will be working with communities right around this Bay to ask and explore some important questions, such as these:
If we take each of those questions in turn (as we plan to do) and really talk together about how we make society and therefore our health and wellbeing better for everyone, rather than leaving it to others to make those decisions from on high for us, then I think we will achieve more than we could ever imagine possible. It is in discovering one another, in encountering the other that we can be transformed and find new ways forward together.
A people movement or social movement such as this will invigorate and create space for those within the systems not only to reconnect with our own humanity but enable us also to have braver conversations about how we can share our resources more effectively, work together more creatively and reimagine how we can provide the kind of health and social care that makes sense for the needs of the people we serve. We might not save £50 million, but we can’t continue with things as they are and if we talk and work together, we could make a really difference.
Here is a video about a brilliant couple of days a bunch of us had in Morecambe, talking about how we discover what it is to be healthy and be part of a social movement to improve the health and wellbeing of everyone:
The subject of this blog is sensitive and difficult. It may stir up some difficult issues or memories for you, as you read. If this happens, then please take time to seek the help you need. I believe this blog and ones to follow might be some of the most important I have written to date.
 I am currently reading a phenomenal book, sent to me in the post, by a dear friend of mine, who is a trained counsellor and knowing the work I do, felt that I should read it also. The book is called “The Body Keeps the Score” by the eminent Psychiatrist, Bessel Van Der Kolk. In my humble opinion, it should be compulsory reading for every person training in any of the clinical specialities, including public health and for those working in education. The book focusses on the detailed research and work done by Van Der Kolk and others at Harvard over the last 30 years in the whole area of Complex Post Traumatic Stress Disorder (CPTSD), or “Disorders of Extreme Stress, Not Otherwise Specified” (DESNOS). It is not a part of our vocabulary, unfortunately, because even now, after a huge evidence base and many studies, there still remains no such psychiatric diagnosis. However, it is a hidden epidemic affecting huge numbers of our population and is the root of many of our major public health issues. So what causes this problem and just how wide spread is it? The evidence shows so strongly that the cause of CPTSD or DESNOS is Adverse Childhood Experiences, which we more starkly call Child Abuse.
I am currently reading a phenomenal book, sent to me in the post, by a dear friend of mine, who is a trained counsellor and knowing the work I do, felt that I should read it also. The book is called “The Body Keeps the Score” by the eminent Psychiatrist, Bessel Van Der Kolk. In my humble opinion, it should be compulsory reading for every person training in any of the clinical specialities, including public health and for those working in education. The book focusses on the detailed research and work done by Van Der Kolk and others at Harvard over the last 30 years in the whole area of Complex Post Traumatic Stress Disorder (CPTSD), or “Disorders of Extreme Stress, Not Otherwise Specified” (DESNOS). It is not a part of our vocabulary, unfortunately, because even now, after a huge evidence base and many studies, there still remains no such psychiatric diagnosis. However, it is a hidden epidemic affecting huge numbers of our population and is the root of many of our major public health issues. So what causes this problem and just how wide spread is it? The evidence shows so strongly that the cause of CPTSD or DESNOS is Adverse Childhood Experiences, which we more starkly call Child Abuse.
Child abuse falls into four main categories: Physical abuse, Sexual Abuse, Verbal Abuse and Emotional abuse – usually in the form of neglect. 10% of children suffer regular verbal abuse. 25% suffer regular physical abuse. 28% of women and 16% of men have suffered sexual abuse. 16% regularly watch domestic violence. 87% of all those who suffer one type of abuse, are also abused in other ways. Each of these forms of abuse lead to major health problems later in life and studies are showing that it is not just mental health issues (many of which lead to inappropriate diagnoses like Borderline Personality Disorder or Bipolar Disorder and ineffective treatments) but also major physical health problems. Those who have been abused are twice as likely than others to develop cancer and four times as likely to have emphysema. The more difficult a person’s experiences, the higher the chance of developing heart, liver or lung disease at an early earlier age with much higher chances of taking more health risks with smoking, becoming overweight or having multiple sexual partners. There is good evidence to suggest a link with autoimmune diseases, such a lupus, and other complex conditions like chronic pain, chronic fatigue and fibromyalgia. The body cannot be separated from the mind and literally keeps the score of the internalised turmoil. So, even if the abuse happens before memories are formed, or our minds manage to forget or block out what has happened, the body simply cannot forget and sometime and in someway, the damage will show itself. Studies show that the overall cost of this appalling reality far exceed those of cancer or heart disease. In fact, eradicating child abuse would cut depression rates by over 50%, alcoholism by 66% and suicide, IV drug use and domestic violence by 75%. Antidepressants and antipsychotics are now some of our largest prescribing costs. We know this, but are doing very little about it. Perhaps it feels too big. Perhaps we don’t want to face the demons involved. Instead, we are numbing the problem, trying desperately to get people to be just functional enough to keep on serving the needs of our economic system, but we are not facing up to or dealing with this horrific problem, nor its true cost.
lead to major health problems later in life and studies are showing that it is not just mental health issues (many of which lead to inappropriate diagnoses like Borderline Personality Disorder or Bipolar Disorder and ineffective treatments) but also major physical health problems. Those who have been abused are twice as likely than others to develop cancer and four times as likely to have emphysema. The more difficult a person’s experiences, the higher the chance of developing heart, liver or lung disease at an early earlier age with much higher chances of taking more health risks with smoking, becoming overweight or having multiple sexual partners. There is good evidence to suggest a link with autoimmune diseases, such a lupus, and other complex conditions like chronic pain, chronic fatigue and fibromyalgia. The body cannot be separated from the mind and literally keeps the score of the internalised turmoil. So, even if the abuse happens before memories are formed, or our minds manage to forget or block out what has happened, the body simply cannot forget and sometime and in someway, the damage will show itself. Studies show that the overall cost of this appalling reality far exceed those of cancer or heart disease. In fact, eradicating child abuse would cut depression rates by over 50%, alcoholism by 66% and suicide, IV drug use and domestic violence by 75%. Antidepressants and antipsychotics are now some of our largest prescribing costs. We know this, but are doing very little about it. Perhaps it feels too big. Perhaps we don’t want to face the demons involved. Instead, we are numbing the problem, trying desperately to get people to be just functional enough to keep on serving the needs of our economic system, but we are not facing up to or dealing with this horrific problem, nor its true cost.
What can be done in the face of such evil? How can we develop a culture of compassion and restorative justice in which we can find a new way through for humanity? It isn’t getting any better. It is just as widespread and far reaching in its consequences as it was a generation ago. Is it possible for us to face up to the startling reality we face? Van der Kolk offers much hope, but it is not within the gift of the health service and social services to tackle this alone. If we are to take this issue seriously, we must embrace what Bessel refers to (at the end of chapter 2) as four fundamental truths:
culture of compassion and restorative justice in which we can find a new way through for humanity? It isn’t getting any better. It is just as widespread and far reaching in its consequences as it was a generation ago. Is it possible for us to face up to the startling reality we face? Van der Kolk offers much hope, but it is not within the gift of the health service and social services to tackle this alone. If we are to take this issue seriously, we must embrace what Bessel refers to (at the end of chapter 2) as four fundamental truths:
 People can be healed of trauma. We need this at both an individual and corporate level. We have become so focussed on saving money, on quick fixes to ensure the NHS and Social Care System can survive, but we are ignoring the root cause of many of our ill health issues. If we are willing to face up to the truth of child abuse in our society and its long lasting and far reaching impact on overall health and wellbeing, then we might just be able to find a way through to healing and restoration of what has become an extremely broken society. In the blogs that follow, I will look at some of the ways we might find a way through this crisis of epidemic proportions. One thing we must face straight away is that we are spending our resources in the wrong places and are focussing our attention in the wrong areas. We must protect our children and help people learn how to be good parents. We must strengthen our school teachers and sense of community. We must invest in the first five years of life far more than we are doing so currently, especially those key first 12 months of bonding and attachment. Together, if we want to, with love, care, bravery and determination, we can change the future. There is hope. There is healing. Our systems are not yet designed to cope with this, but we must speak the unspeakable, break the silence and face up to the truth. The truth will set us free and enable us to develop the kind of wellbeing that every human being should be able to live within.
People can be healed of trauma. We need this at both an individual and corporate level. We have become so focussed on saving money, on quick fixes to ensure the NHS and Social Care System can survive, but we are ignoring the root cause of many of our ill health issues. If we are willing to face up to the truth of child abuse in our society and its long lasting and far reaching impact on overall health and wellbeing, then we might just be able to find a way through to healing and restoration of what has become an extremely broken society. In the blogs that follow, I will look at some of the ways we might find a way through this crisis of epidemic proportions. One thing we must face straight away is that we are spending our resources in the wrong places and are focussing our attention in the wrong areas. We must protect our children and help people learn how to be good parents. We must strengthen our school teachers and sense of community. We must invest in the first five years of life far more than we are doing so currently, especially those key first 12 months of bonding and attachment. Together, if we want to, with love, care, bravery and determination, we can change the future. There is hope. There is healing. Our systems are not yet designed to cope with this, but we must speak the unspeakable, break the silence and face up to the truth. The truth will set us free and enable us to develop the kind of wellbeing that every human being should be able to live within.